The surgical repair of pars interarticularis fractures is now possible with new technology. Internal fixation of the fracture has improved dramatically with new O-Arm and Stealth visualization (see website on this technology). A surgeon can safely place a screw directly across the fracture site, which rigidly fixes the fracture and significantly improves healing potential. The use of bone morphogenic protein (BMP), a synthetic protein that induces the patient’s own stem cells to turn into bone healing cells speeds up the healing process and increases success rate of fusion.
The surgical repair typically takes about 3-6 months to unite. There are rare patients that can take up to a year to heal. During that period of time, the patient will need to wear a brace and reduce normal activity. Bone healing uses the same mechanical principles with a surgical repair as with a fracture left to heal on its own. The difference is that with surgery, there is solid internal fixation to make the repair rigid while the bone attempts to heal.
The healing environment also has been significantly improved. Before surgery, cartilage and fibrous tissue existed in the fracture gap between the broken fragments that prevented healing. After surgery, the fractured bone ends are cleaned of the soft tissue debris and coopted end to end. Bone graft and BMP are both placed into and around the fracture gap to induce healing potential.
Are you a candidate for surgical repair of a pars interarticularis fracture?
Would you like to consult with Dr. Corenman about your condition?
You can set up a long distance consultation to discuss your
current X-rays and/or MRIs for a clinical case review.
(Please keep reading below for more information on this treatment.)
Which patient is a candidate for ? If the patient has significant degenerative disc disease or a significant slip of one vertebra on the other, he or she would most likely not be a candidate for fracture repair. What about the patients with pars fractures and no symptoms?
This is a treatment conundrum. Some adults with bilateral pars fractures do not develop lower back symptoms in their lifetime. The question then rises if surgeons should surgically repair the non-healed pars fractures in asymptomatic children. There is not a perfect answer to this question. Athletic children do seem to have a higher incidence of lower back pain with pars fractures which leads to repair but that does not necessarily mean that every athletic child needs a surgical repair.
Most individuals with bilateral pars fractures will develop degenerative disc disease. Many will also develop a slip of one vertebra on the other (an isthmic spondylolysthesis). A good percentage of patients will develop pain and some will have disabling pain. What would be the total percentage of disabled patients with an isthmic spondylolisthesis? That information is not fully known at this point.
It is predicted that a surgical repair in the child with a spondylolysis, no slip and no degenerative disc disease will prevent the degenerative cascade that so commonly proceeds after a non-healing pars fracture. The biomechanics of the repair makes sense and to see older patients with the symptoms of a painful isthmic spondylolisthesis requiring fusion makes prevention and repair a reasonable course of treatment. However, there have not been enough pars fractures repaired and followed out long enough to see if this prediction of degenerative prevention is correct. Pars repair could eventually become the standard of care in children.
If degenerative disc disease sets in or there is a significant slip (spondylolisthesis– not spondylolysis), the surgical repair of the pars fractures may be ineffective in relieving lower back pain. A fusion may be necessary to give pain relief. The tests to determine what course of action should be performed are an MRI and a subsequent discogram (see section on discogram on this website)
For more information on please contact Dr. Donald Corenman, spine surgeon and back specialist offering diagnostic and surgical second opinions to patients in the USA and around the world.
Related Content

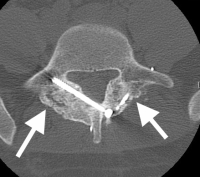
(Click to Enlarge Image) CT scan of pars fracture of L5. White arrow points to fracture. Thisadolescent had 4 months in brace and continued to have pain upon return toactivity.
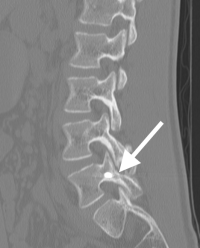
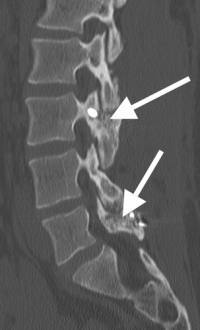
(Click to Enlarge Image) CT scan of healed pars fracture. White arrow points to healed fractureWhite dot in bone is tip of screw used for repair.

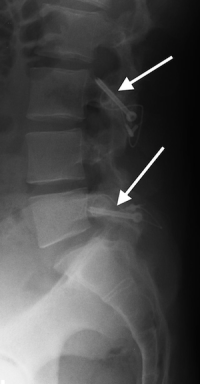
(Click to Enlarge Image) X-ray of pars repair. Note the screw through one side of pars and thewire tightening the other side.
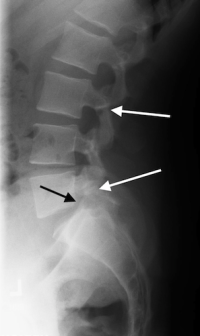
(Click to Enlarge Image) Lateral X-ray of pars interarticularis fractures of L3 and L5 in a 15year old boy who has fail. Black arrow points tominimal slip of L5 on S1. The MRI notes a normal disc at that level.