What is a Lumbar Discogram?
The discogram is a unique spinal test. It is the only test to indicate if the disc is the source of lower back or neck pain. The discogram test actually stresses the disc to determine if it is reproducing pain. This test also has a visual component to it. You can observe what the architecture of the disc is like by the discogram to corroborate the stress results.
Most spinal injection tests are analgesic. These tests “numb” a structure and the pain level in the patient will be temporarily reduced for 2-3 hours. The discogram is the only spinal test that is provocative. It is designed to reproduce pain in an awake patient to prove the source of pain or the “pain generator”. The pain is replicated only for an instant and if pain is reproduced, the patient can identify if the pain is the typical pain that occurs from day to day.
How Does a Discogram Work?
The concept of the discogram is easy to understand. Back pain from the disc is caused by aggravation of pain receptors in the torn annulus (plies of the tire) or the compression of a degenerative bony vertebral endplate (see degenerative disc disease of cervical or degenerative disc disease lumbar spine in separate section). This test is designed to stress these structures and reproduce the normal day to day pain only for a moment. It is essentially a pressure test of the disc designed to reproduce typical pain.
The test also has value in looking at the morphology of the disc (what the inside of the disc looks like). The fluid injected is X-ray contrast dye (mixed with some antibiotic). If tears are present, this dye will demonstrate the tears in the disc walls. The walls will be either intact (the dye looking somewhat like a cotton ball in the center of the disc) or there will be a disruption of the disc wall. A through and through tear will leak the dye into the surrounding tissues.
How is a Discogram Performed?
The test is actually very simple. A needle is placed into each disc in question in a sedated patient. Only after needle placement, the patient is awakened. If you have ever had an IV placed, you will know that the only discomfort occurs when the IV is initially placed. After the IV is in, there is no lingering pain. Just like getting an IV placed, the discomfort of needle placement only occurs with the initial needle positioning and that discomfort is never noted with proper initial sedation.
It is a very investigator sensitive test. That is, the physician who leads the examination (normally an anestheologist, an interventional radiologist or a PM & R physician) has to be meticulous where he or she places the needles. The location of the end of the needle is paramount. The needle tip has to be placed into the center of the disc directly in the nucleus (jelly of the donut). If the needle is positioned in the layers of the annulus, the test will cause pain, even in a normally non-painful disc. Also, the patient has to be reasonably awake and alert during the provocation while still under minimal sedation. A patient who is too sedated will not be able to confer accurate information.
The test should be “blinded” to the patient. For more accuracy, the discographer should test the discs in non-sequential order that is not communicated to the patient and hide the fluoroscopy screen from the patient’s view. If L3-S1 were being tested, the order should be “mixed up”. For example, test L3-L4 first, L5-S1 second and L4-L5 third. This assures the patient cannot know which segment is being tested and give what he or she thinks is the “appropriate” results. If there is any doubt about the patient’s genuineness regarding the origin of his or her back pain, this takes some of the question of origin of pain out of the picture.
There are rare cases of patients that are allergic to X-ray contrast dye and if necessary, these patients will then get a saline discogram. There is no imaging dye that is injected into the disc, so the pain response can be assessed but the integrity of the interior of the disc will not be known. The discographer has to be a master of his craft to be able to do this procedure.
What Do Discogram Results Mean?
The discogram has to generally test more than one disc level. There has to be a “control” or normal disc included in the testing. The levels determined to be tested progress from the MRI and x-ray findings as well as the history and physical examination (See how to read an MRI or Xray). There are three possible results with a discogram. All the tested discs are painful, none of the discs are painful or only some of the discs are painful.
If all the discs including a normal disc are painful, the patient is most likely not a good surgical candidate. This is because the thalamus, an organelle in the lower portion of the brain and the “switchbox” for pain signals cannot distinguish between a normal and abnormal disc. A normal disc may cause some “pressure” discomfort under high pressure but will not be significantly painful. If the discogram has been performed well and normal discs are painful, any surgery has less likelihood of being successful.
If none of the discs are painful, then the spine pain problem probably rests with some other pain generator. Investigation of facet pain, nerve pain or other painful stimuli needs to be completed. There are rare occasions that the disc suspected of generating pain is so torn and disrupted that there is no possibility of generating enough pressure in the disc using the discogram technique. This would be similar to having a massively torn sidewall on a tire where any air pressure put into the valve stem would immediately leak out of the tire and pressure could not be built up. Surgical decision making is more difficult in this case.
Over 90% of the time, the presentation of discogram results would indicate a non-painful normal disc and a painful torn disc or discs. This would point toward the painful disc or discs being the source of lower back or neck pain and the control or normal level indicate that there is no pain processing problem with the brain. Depending on the circumstances, this patient would probably make a good surgical candidate.
There are rare times that there is no normal disc in the area to be tested. All the discs of the area to be tested are degenerative but some more so than others. If there is no disc that is normal on MRI and all develop some discomfort, titration of the amount of pain generated is important. Some discs can cause only minimal pain. Is the pain the same as the patient has day to day? There are some discs that are pain discordant. They create pain but the pain is not recognizable as typical day to day pain.
The decision as to if you are a good surgical candidate will depend upon the discogram results as well as many other variables. The discussion with your surgeon is very important.
For more information on spinal discograms, or for additional resources on orthopedic spine conditions, exams or surgeries, please contact Dr. Donald Corenman, Colorado spine surgeon at 888-888-5310.
Related Articles
- Cervical Discograms
- Epidural Injections and Selective Nerve Root Blocks- Diagnostic and Therapeutic
- Facet Blocks and Rhizotomies
- Diagnostic vs Therapeutic Injections
- Pain Diary Instructions for Spinal Injections
- Home Testing For Leg Weakness
- How to Describe Your History and Symptoms of Neck, Shoulder and Arm Pain
- How to Describe Your History and Symptoms of Lower Back and Leg Pain
- Walking (gait) Disorders
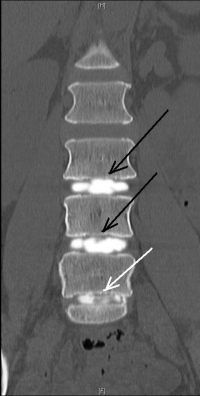
(Click to Enlarge Image) This is a front to back view (AP) of the discogram at L3-4, L4-5 and L5-S1. Again, the black arrows point to the top two normal discs (L3-5) and the bottom white arrow points to the disrupted L5-S1 disc. You can see a tear in the side wall of the lowest disc (L5-S1).
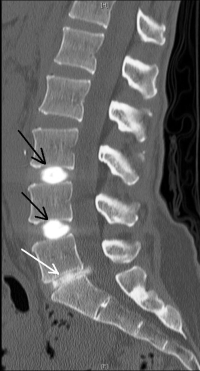
(Click to Enlarge Image) This is a lateral CT scan of a discogram of L3-4, L4-5 and L5-S1. The black arrows point to the top two normal discs (L3-5) and the bottom white arrow points to the disrupted L5-S1 disc. You will notice that the normal discs (L3-5) are thick and hold the dye within the disc with a typical “cotton ball” type pattern. You could see with your minds eye (deduction) that the annular walls are intact and the dye is held within the central jelly. The lowest disc at L5-S1 (white arrow) has a tear in it and the dye is leaking out the back into the spinal canal.
