The first step in treatment of mechanical back disorders is the diagnosis of the pain generator. This will dictate what therapies can be used. This importance cannot be understated.
Certain disorders like lumbar spinal stenosis should have a flat back program (described later in this discussion) while degenerative discpatients need an extension program. Degenerative spondylolisthesispatients need spine stiffening while degenerative disc patients need range of motion.
The final step is how to reverse or ameliorate the problem mechanics and strengthen the associated muscles. This is essence of therapy.
In general, what can be done with mechanical or physical therapy? Therapists can educate patients to strengthen and condition muscles, stretch ligaments and discs and learn better mechanical ways of doing activities (ergonomics). Cardiovascular training also plays a large part in recovery. Muscle strengthening is designed to make the muscle more capable of supporting a heavier load.
Chiropractic manipulation can be helpful to reduce restrictions on vertebral motion or might be contraindicated due to instability of the spine.
Conditioning makes the muscle more resistant to fatigue from repeated stress. Stretching can reduce loads to spinal structures and ergonomics is a way to retrain the body to lift, bend and load the spine that won’t be as detrimental. Restrictions may be in order to prevent painful and destructive loading of the spine.
In sports, there are adjustments to be made to the bike, skis that are designed to be more impact tolerant and binding setting that can be more forgiving. There are shoes that can reduce shock and some sports that may just simply need to be avoided. Hikers can use ski poles to unload the spine, especially when descending a steep grade. Athletes can change their form to minimize impact and torsion on the spine. This includes baseball and basketball players, golfers, football and soccer stars as well as tennis pros and ski racers.
All individuals can strengthen their cardiovascular system (heart and lung conditioning). No matter what the diagnosis, cardiovascular training has been demonstrated to significantly help with pain reduction as well as allowing muscles to work longer without becoming fatigued. This is a must for spinal rehabilitation.
Even with disabling back conditions, there is a cardio-exercise that can be adapted to allow conditioning without triggering pain.
This discussion is not a cookbook. It does not give advice on how many repetitions of what specific exercise needs to be done to strengthen what particular muscle. This section explains the biomechanics, gives guidelines on what mechanical changes need to be done to alter the stresses and the general way to do it. As has been noted, a skilled and knowledgeable therapist, no matter what their specialty, is one of the keys to pain relief and better function.
Video Lecture on How to Identify and Treat Lumbar Spinal Disorders
Core Strengthening
If there is one key phrase used to describe back pain rehabilitation, it is “the core”. There is good reason for this. The reason core muscles are so important is that they are one of the major keys to stabilize the spine no matter what the diagnosis is. Every single disorder found in this chapter will benefit from core strengthening. Since discs can’t be made stiffer any other way (unless the patient undergoes surgery or awaits father time for further degenerative changes), the core muscles can be strengthened to help control the abnormal motion of the disc.
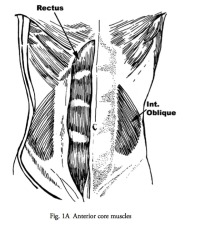
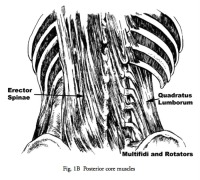
Think of the lumbar spine as bunch of loosely joined building blocks. The muscles that directly insert into these blocks are small and have poor strength. That is, they can’t generate the necessary forces to restrain abnormal movements of the spine. The long (and strong) extensor muscles of the back don’t directly attach into the lumbar spine vertebra so they can’t individually affect stability. They do however attach into all the surrounding bony structures to give group (or core) stability.
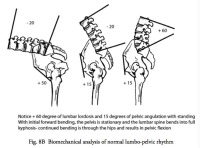
(Fig. 1 A&B)
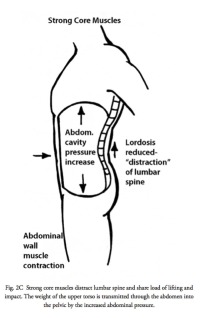
Now when the core is strong, muscles actually work against each other to stop motion of the spine, essentially “splinting’ the spine. This is similar to the elbow. To make the elbow stiff when holding a heavy object, one can contract both the front and the back muscles of the arm (biceps and triceps) to stabilize the joint. The same thing can be done to stabilize the spine.
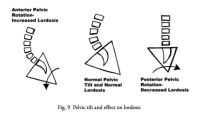
Contraction of the anterior and posterior muscles at the same time immobilizes the core by increasing the abdominal pressure through the anterior muscles and compression of the thoracic spine onto the pelvis with the posterior extensor muscles.
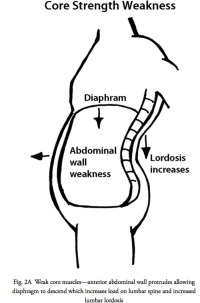
The abdominal contents act like a giant water balloon entirely wrapped by a boa constrictor. Contraction of the abdominal muscles increases pressure in the belly, which is opposed by the pelvic floor below and the diaphragm above which stiffens the lumbar spine even more. (Fig. 2A,B,C)
I will not endorse any specific program as a great therapist may come from many different types of schools. However, if there is one set of exercises that is generally helpful in most situations, it is “Pilates”. These series of exercises are some of the most consistent endeavors to achieve a strong core. Mind you, there are many other techniques that can also strengthen the core.
One important fact- muscle strengthening takes time for results to occur. The differences from week to week are not easily noticeable and the progress can be frustrating. Patience and the consistency of performing these exercises are the basis to increasing strength and stability. At least two and probably three months of strengthening with unswerving work on the core will be needed before a noticeable difference can be seen.
Strength without Injury
Any muscle can be strengthened with the appropriate amount of work. One of the keys is to strengthen muscles without hurting the structures they protect. Anyone can go to the gym, get involved in an aerobics class and weight room and gain strength and endurance. If that individual has a symptomatic disc or a spondylolysthesis however, many exercises will be painful. A patient will be discouraged by performance training only to have increased pain after the exercises. This is where a good therapist comes in. A well-trained therapist can design a program that will not be harmful, and still lead to strength and conditioning.
Lever Arms and the First Rule of Physics (Ergonomics)
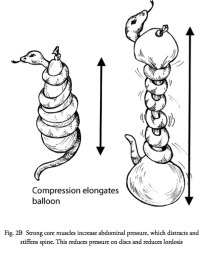
One of the problems with the lower back muscles is that they are at such a mechanical disadvantage. If we look at a simple diagram of spinal biomechanics, remembering basic physics and principles of lever arms, the force generated by bending forward and lifting has to be resisted by an exact opposite force. This opposing force is generated by the pull of the back muscles and the dampening restraint of the ligaments and discs.
As may appear obvious, you can see that the heaver the load, the more stress occurs to the lower back. What is not immediately obvious is that the farther away the load is from the body, the more stress is generated to the back. Also, the more bent forward, the more Archimedes principle of levers and fulcrums comes into play. The torso and upper extremities make up the lever arm. Therefore, the further the individual bends forward, the longer the lever arm becomes and therefore the greater the strain on the back. (Fig. 3A&B)
This is where ergonomics plays an important role. The simple act of lifting can be made much less damaging to the spine by bringing the load much closer to the body and keeping the back flat while bending the knees. Use the knees to lift as the quadriceps muscles are very strong.
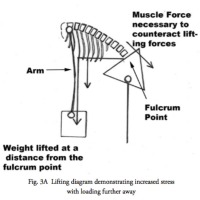
Avoid Bacon, Lettuce and Tomato (BLT)
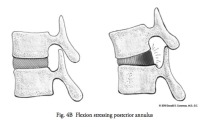
There are many positions that can load the spine that are not healthy for the discs. The discs “abhor” rotation (twisting or lateral bending) as it puts them at a mechanical disadvantage. When one twists, 50% of the fibers of the disc are relaxed and the other 50% are put under significant load. Then, with a forward bend, all the tension is put on the posterior part of the disc, which further increases the stress on the already overloaded fibers. Combine a twisting motion with a forward bend and then a lift and the perfect environment for an annular tear has been created. (Fig. 4A&B)
Unfortunately, many people lift this way. This is a learned behavior as this is the easiest way to move an object with the least expenditure of energy (but the most strain on the back). This is all fine and good if the individual is young and the disc is resistant to tear but with any aging or genetic predisposition, this is a recipe for injury. Patients have to relearn how to lift to avoid this position (the BLT position- Bending and Lifting whenTwisting).
Hamstring Stretches
The hamstring muscles typically do not get stretched in our society (we don’t squat or sit on the ground). This leads to hamstring contractures.
The hamstrings tend to tether the pelvis when they are contracted. The act of bending forward consists of motion of both the hip joints and lower back. Actually there is more motion in the hips for forward bending than in the lumbar spine (in a two or three to one ratio). (Fig 5)
If the hamstrings develop contraction, they will not allow the pelvis to bend and more pressure is brought upon the lumbar spine. The moral of this story is to stretch the hamstrings to prevent lumbar spine stress and pain. There are hamstring stretching exercises on this website.
Back Braces
Back braces can be very helpful for pain syndromes. What these braces all do is compress the abdomen to make the back more rigid- just like the diagram above of the snake compressing a water balloon. The problem with these braces is that they make the abdominal muscles weaker over time.
Instead of contracting these muscles to make them stronger, the individual wearing a brace actually pushes their belly into the brace, which is the exact opposite maneuver as a core-strengthening program. This obviously weakens the core muscles.
These braces do work for lifting but should only be tightened immediately before the lift and then released when the lift is over.
I put patents into this brace after lumbar surgery to “rest” the back muscles. The pressure on the back and belly is also a good reminder to reduce motion while the spine heals.
Treatment of Specific Diagnoses
Annular Tears
This is an acute injury. It may seem like a simple “give” in the lower back at the time, but if there is an inflammatory response, the patient may be incapacitated. With a simple tear, the symptoms will disappear within 2 days to as much as 6 weeks and generally will cause no further problems. This is called a self-limiting injury as it will generally fade away with time. There are treatments that can reduce the symptomatic period.
A back brace or corset makes the patient comfortable. Physical therapy modalities such as electrical muscle stimulation, massage and ultrasound can reduce the spasms. Chiropractic manipulation if done carefully can also reduce muscle spasm. Medications such as pain-killers, NSAIDs and muscle relaxants are helpful. With severe pain and spasm, consideration of a short-term oral steroid should be given.
Obviously, significant reduced activity goes hand in hand with severe pain and spasm. 1-2 days of bed rest may be in order at the severe onset of pain but should be avoided as soon as the patient can ambulate. Epidural injections in the most painful cases can be helpful, but this may require an MRI prior to the injection.
Degenerative Disc Disease
The key for treatment of degenerative disc disease is to think in terms of management. As has been noted before, discs don’t heal so self-care needs to be a lifetime affair. This is actually not as much a perceived problem as it seems as a successfully treated patient will be stronger and fit. If the home exercises are not continued, eventually the muscles become weaker, old bad habits rear their ugly head and the symptoms may reappear.
For acute flair-ups, the same treatment as an annular tear noted above is in order. For chronic symptoms, stretching, strengthening and conditioning are important. Stretching is importantly to perform slowly. A slow gentile continuous stretch is more therapeutic than a bouncing type stretch. In general, degenerative discs won’t become more mobile with stretching (that would not be beneficial) but improvement of the motion of the surrounding discs will improve which in turn takes the stress off the painful one.
Hamstring muscles are commonly tight with degenerative disc disease and this tethers the pelvis. Tethering the pelvis makes it unable to act as a shock absorber and the lumbar spine sees more stress. An absolute to reduce spine discomfort is to stretch the hamstrings every night until you can come close to touching the toes.
As will be repeated ad nauseum in this chapter, core strengthening is the key to improvement and pain relief. The core muscles are the best way to splint the lumbar spine and reduce stress on the discs. Start with pure isometrics for a very deconditioned core (strengthening with no motion of the spine) and advance to isotonics (strengthening with motion) when the muscles have developed some endurance.
Medications can be very helpful. The list is similar to annular tear treatment protocol but oral steroids are not used unless there is a severe flare-up. Narcotic medications need to be used judiciously.
In general, back corsets or braces should not be used as these tend to weaken the abdominal muscles. Instead of contracting these muscles to stabilize the spine, patients tend to push out against the corset, weakening the abdominals when the brace is not in use.
There are exceptions to this rule. Weight lifting belts are helpful for motorized impact sports like off-road motorcycling and snowmobiling. Skiers can also benefit occasionally. With jobs requiring heavy lifting on an intermittent basis (contractors, etc.), a belt can be worn loosely and tightened only when a heavy load is encountered.
In sports like mountain biking where aerobic physical activity is paramount, the belts are contraindicated as these belts will prevent flexion and restrict the diaphragm.
Ergonomics
In general, individuals with degenerative disc disease will not like flexion activities. Bending forward loads the painful disc and many get relief with extension (bending somewhat backwards). An exception is cycling, as bending forward is ameliorated by bearing the weight of the upper body on the handlebars.
Sports activities can be modified to reduce stress on the lower back. A classic example is the golf swing. Reducing lumbar rotation and using the shoulders and pelvis more can reduce the stress on the lower discs. With bicycling, shortening the stem and increasing its height can significantly reduce stress. A seat post that is too high can cause pelvic rocking which stresses the discs.
Running is more difficult to modify, but with shoes that have viscoelastic soles and insoles to reduce shock and running on dirt and grass vs. a paved course can help. Long hikes can stress the discs and fatigue the core muscles. Hiking poles can reduce impact to the lower back and have an extra benefit of allowing greater upper body conditioning
Skiing can be improved with a more shock absorbing style and skiing on surfaces that are not as hard packed to reduce stress. A softer ski reduces impact and converts less stress to the lumbar spine. The DIN setting for ski binding release can be reduced. This insures a softer skiing style as a more aggressive style will overload the spine but cause a premature release, reinforcing a softer style.
Swimming is a wonderful form of exercise for severe DDD. It is non-weight bearing, unloads the spine and is performed in extension, further reducing pressure on the disc.
Occupation can be modified somewhat. Some occupations however require heavy and awkward lifting which degenerative changes in the back may not be able to withstand. However, understanding lifting mechanics may reduce load enough to make the job tolerable.
The workplace can be modified to reduce stress on the spine. With standing, such as the occupation of bank teller, a step stool under one foot with alternation of the upward leg can reduce the pressure on one area and make standing more tolerable. Padded floors or mats can reduce standing pressures to relieve back pain.
Sitting positions can be modified to allow more or less lordosis, flexed forward position or somewhat extended. Wedges can be used on the seat to increase or reduce lordosis. The computer terminal can be raised or lowered depending upon the disorder.
A “Balans” or kneeling type chair will increase the lumbar lordosis and reduce disc pressure. Simply using an exercise ball for sitting at a desk reduces disc pressure, allows for motion to prevent jelling of the muscles and contributes to stronger core muscles. The individual must balance while they sit. Just make sure the ball doesn’t suddenly deflate or puncture.
Romance and Your Back
There are positions that can aggravate the back when in a romantic mood. Pelvic rocking involves significant extension of the spine, a problem for stenosis, spondylolysthesis and facet disorders. Standing involves flexion, which loads the discs, not the best position for degenerative disc disease. Imagination to discover positions that will not load the spine in a painful manner is the order of the day.
Continued Degenerative Changes
Now for some good news. Over time, the discs become more degenerative. Yes, this is good news. The more degenerative a disc becomes, the stiffer it is. The stiffer it is the less motion can occur. Since motion causes pain, as the disc stiffens, the back generates less pain. The problem is, no one can predict how long it will take for the disc to stiffen and not all discs become stiff with age. The exception is isolated disc resorption (IDR).
Isolated disc resorption (IDR)
This disorder includes all the problems of DDD above with the problem of significant aggregation with impact and load. For this particular disorder, core strengthening is important but activity restriction is equally as important. There is no way to help cushion the impact of some activities and these actions may simply need to be eliminated. Many individuals can still swim, ride a bike (with seat and handlebar adjustment), play golf, swim and even get into the gym to lift weights with the right body mechanics. Most successful treatments follow the degenerative disc protocol.
Facet disease
Physical therapy and chiropractic can be effective in treating painful degenerative facets. Facets are loaded when bending backwards therefore activities that cause extension creates pain. The serve or overhead in tennis, swimming, volleyball and any overhead activity such as painting the ceiling can increase pain. Rotating the pelvis backwards flattens out the spine and reduces pressure on the facets. (Fig. 6)
Strengthening the posterior rotators will rotate the pelvis backwards. The muscles involved are the abdominals and gluteal muscles as well as the hamstrings. There are times when mobilization is not beneficial as a degenerative facet may correlate with a degenerative spondylolysthesis. Mobilization of this segment may worsen the slip of the vertebra so chiropractic treatment may be contraindicated.
Sacroiliac Joint Dysfunction
The primary concern here is whether the correct diagnosis has been made. So many times, the sacroiliac joint is an innocent bystander for referral pain from the L4-S1 region. If a true SI disorder, treatment includeschiropractic manipulation, physical therapy modalities and prolotherapy. In general, injections of steroid give good diagnosis relief in most cases. In resistant cases, the other therapies can be very helpful. Muscles really don’t cross this joint, so muscular strengthening is not very effective. Prolotherapy is the injection of an irritant into the SI joint to stiffen the joint, kill the pain receptors and reduce pain.
Treatment for Leg Pain
Herniated Disc
The major theme early in the treatment of sciatica is to avoid a flair-up of the nerve. The therapist has to be careful with the “straight leg raise” maneuver as this can really irritate the nerve root. Extension and neutral spine exercises are the order of the day. Most herniations are located at L4-L5 or L5-S1 so the sciatic nerve is involved. If the herniation is higher (L3-4 or above), the femoral nerve will be involved and these rules will be reversed.
Only when the nerve is less inflamed and can be gently stretched can leg flexion exercises be started. If the therapist stretches the nerve too much, especially in the early stages, a recurrence of the leg pain can occur. The therapist however does eventually have to start stretching the nerve. Occasionally, the nerve can become irritated even with a gentile stretch. This is truly where the “art” of treatment comes in.
In therapies for these radiculopathies, the care-giver needs to strengthen the core muscles, gently stretch the nerve without aggravating it and treat any trigger points that are caused by the nerve compression. Trigger points are discrete tender points normally found at motor points in muscles that cause local spasm and discomfort. Continued cardiovascular training during therapy is essential to reduce pain and make existing pain more tolerable.
Medications are quite useful for early control of the pain and spasm. If the nerve is really painful, even strong narcotics won’t dull the throbbing. This is where an epidural steroid injection is very valuable. After the injection, there can be immediate relief and the relief can be long standing. It may however take three to six months or longer for certain activity restrictions to be lifted to prevent root pain recurrence. Membrane stabilizers can be effective for severe pain
Foraminal Stenosis, Lateral Recess Stenosis and Central Spinal Stenosis
All of these stenosis conditions will be aggravated by exercises that cause the back to extend (bend backwards). This is much more common than you might think. The simple act of standing up causes the back to bend backwards which will aggravate these conditions.
Therapists should work on pelvic “tucks” or the flat back position for standing. That is, to flatten the lower back by tucking the pelvis in (rotating it posteriorly) to increase the room for the nerves. This is performed by strengthening the abdominal muscles and the hamstrings. This is the same therapy as the treatment of facet disease. (Fig. 6)
The same conditions hold for sports and activities. Again, basic core strengthening and endurance training is important. Walking and hiking can be helped with ski poles to allow forward bending, especially with walking downhill.
Ergonomics of Foraminal Stenosis and Spinal Stenosis
What is interesting is that stenosis patients can normally snow ski all day. As is well known, a good skier will force his or her weight towards the front of the skis. This requires forward flexion, the maneuver that opens the canal and gives perfect relief for the stenosis patient. These individuals will not however, like to stand in lift lines. The ski boots force the lower leg into a forward lean. To compensate when standing in the lift line, the patient needs to lean backwards, the exact position these patients need to avoid. If you look at these skiers while waiting for the lift, they will lean forward on their poles.
The same is mechanism is noted with bicycling. Again, a forward lean on the bike opens the spine and these individuals can bike all day long. In fact, a differential test can be used for these patients without an MRI available. Have the individual pedal on a stationary bike for 10 minutes. This should be no problem. Then have them do 5 minutes on a flat treadmill. They will develop symptoms of claudication. Note that if the treadmill is significantly elevated, they will need to bend forward to keep balanced. This could give them enough decompression to negate the test.
“Piriformis Syndrome“
This is a very rare syndrome and as uncommon as the sacroiliac joint causing pain. The first order of business is to be sure the diagnosis is correct. If so, stretching of the muscle is paramount. Local treatment in the form of ultrasound and massage can be helpful.
Isthmic Spondylolysthesis
The first important task is to diagnosis the fracture if the patient is young. Any chronic lower back pain in a young individual has to be considered an acute pars fracture unless proven otherwise. The injury is diagnosed by x-rays, a CT scan and or a bone scan. Treating the impending fracture as soon as it starts to occur in the young is important as this is the best chance for healing.
Treatment starts with reducing the stress on the bone by wearing a flat back brace. Activity restriction helps to take the load off the bone to allow healing. However, even with the best of treatment, some of these impending fractures still won’t heal.
Even when the fracture is established and has not healed, many of these patients still do not become symptomatic. This is a recurring theme in spine disorders. The individuals that develop pain develop it much later in life and are uncovered by an episode that aggravates the defect. If patients do develop late pain, it can become a difficult condition to treat.
Late treatment is based on pelvis rotation and strength to stiffen the lower back (sounds like the treatment for facet disease and stenosis- doesn’t it). This condition can be helped by “tucking” the pelvis (rotating it posteriorly) to flatten the sacral angle. This positioning reduces the forces on the slip.
Again core strengthening is paramount. Here, the therapist does not want to stretch the lower back, but to reduce motion of the L5-S1 segment. Motion of the lumbar spine is undesirable as the goal is to stiffen the slip area, not mobilize it. Stretching the hamstrings is a must as these are chronically tight. Stretching muscles next to a structure you don’t want to mobilize is a big order to fill. Again, this ability defines a great therapist.
Degenerative Spondylolysthesis
Patients with stenosis will unconsciously try to keep their back flat when they walk to keep the canal as open as possible. The only ways to do this are to rotate the pelvis posteriorly or to bend forward. Bending forward while walking wastes too much energy from muscle contraction. To compensate for this, many will keep their knees bent while walking. This is still very inefficient, but better than the alternative.
Therapy for this condition focuses on core strength (again) but here, posterior pelvic rotation is paramount. Stretching the pelvis while avoiding stretching the slipped vertebra is important. Strengthening and conditioning the abdominals and hamstrings while stretching the psoas muscles keeps the posterior pelvic alignment. If the pelvis won’t posteriorly rotate enough, strengthening the quadriceps muscles to allow a bent knee gait will be helpful.
Scoliosis
For adults, treatment of degenerative scoliosis is really the treatment of whatever painful degenerative components occur. Controversial is whether to put scoliosis patients into a stretching or yoga program. On one hand, stretching contracted painful structures will give some relief. On the other hand, scoliosis patients will benefit from avoiding stretching as avoidance will allow the spine to become stiffer as this will prevent progression of the curve. Progression of the curve can compress a nerve root or allow the deformity to become greater, triggering the need for surgery.
The treatment of children with idiopathic scoliosis is really a much different discussion. Children’s scoliosis is non-painful. In fact, this is the reason there are scoliosis screenings in school. The purpose of treatment in young individuals is to reduce the progression of the curve. Kids with a certain degree of curve will increase the size of the curve with growth. Brace treatment is designed to prevent the curve from increasing.
Thoracic Hyperkyphosis
An increased thoracic curve needs to be compensated by an increased lumbar lordosis. This increased lordosis can cause increased strain on the facet joints and premature wear. Standing and loading the spine (lifting and impact) will increase low back pain.
Treating only the lumbar spine will not reduce the stress on the spine. The thoracic spine also needs to be treated. There is no way to really reduce the increased thoracic kyphosis but strengthening the thoracic extensor muscles and stretching the curve will give some relief. Strengthening the lumbar extensor muscles will help to compensate for the lumbar stress.
Conclusion
As you can see, strength is the key to manage any of these disorders. Core strength and hamstring stretches are paramount. Understanding the particular disorder to know how to load the spine helps to modify the activities you engage in. Specific therapies can reduce load and make the job of daily activity more acceptable.
Related Content
(Click to Enlarge Image) Fig. 2B – Illustration of the effect of strong core muscles on the abdominal contents.
(Click to Enlarge Image) Fig. 3A – The effects of lifting while bending over. This diagram notes the much greater stress on the lower back with forward flexion.
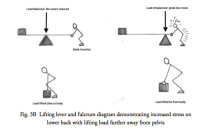
(Click to Enlarge Image) Fig. 3B – This diagram demonstrates the effects on the lower back with lifting further away from the pelvis.
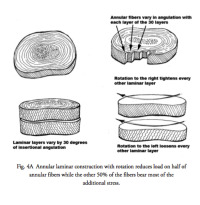
(Click to Enlarge Image) Fig. 4A – This illustration notes the adverse effects of twisting when loading the disc
(Click to Enlarge Image) Fig. 4B – Note that with forward bending, most of the stress on the disc is in the back wall. Add this action to a twist and you can understand the increased stress that occurs with BLT