The lumbar spine is essentially a series of five building blocks called vertebra. They stack up, one on top of the other. They sit on the sacrum, the triangular bone wedged into the pelvis. The sacrum is the “base bone” of the spine. The vertebrae are separated in front by the discs. The discs are the shock absorbers of the spine. They allow motion and yet absorb impact.
The back part of the spine contains the joints called the facets. These facets are the governors of spinal motion. They will allow bending forward, backward and side to side but resist rotation. They also act as door stops to prevent one vertebra from sliding forward on the one below (degenerative spondylolisthesis).
The transverse processes stick out from the sides of the vertebrae and are essentially lever arms that muscles attach to. These levers allow smaller muscles to move the vertebral segments more easily. The spinous processes which project out the back of the vertebra are also lever arms. Strong ligaments attach that prevent the spine from bending too far forward and when bending backwards, these processes abut, preventing too much backwards motion.
Spinal Canal
The bony spinal canal sits in the center rear of the spine. It contains the spinal cord (which actually ends at the upper lumbar spine) and the nerves that exit out of the spinal cord (called the “cauda equina”- Latin for “horse’s tail”). You can think of the spinal cord as an elongation of the brain. It is as sensitive to injury as the brain and has some functions similar to the lower end of the brain (the brain stem). The biggest difference is that the brain is housed in a rigid bony cavity for protection and the spinal cord is housed in a moveable structure (the spinal column) that can and does wear out. This wear causes bone spurs and disc herniations that can compress the cord and therefore interfere with its function.
The nerves in the lumbar spine below the end of the cord are all peripheral nerves, not central nerves. Peripheral nerves in general are much more resistant to compression and can heal if injured whereas the spinal cord generally doesn’t. This fact comes into play if an injury is at a higher vs. a lower level in the lower back.
As always there is one exception. There is a small filamentous set of nerves called “Nervi Erigantes” in the cauda equina. These are the parasympathetic nerves that make the bowel and bladder function. These nerves come right out of the end of the spinal cord called the “conus medularis”. There is one rare emergent condition involving these nerves, usually caused by a large disc herniation called “cauda equina syndrome”, generally a surgical emergency.
The spinal canal changes in diameter and volume with different positions. Bending forward enlarges the canal, making it 20% larger. Conversely, bending backwards makes the canal 20% smaller.
Lumbar Disc
Mechanically, everything in the lumbar spine revolves around the disc. The disc functions like a shock absorber. This structure absorbs impact and still allows for motion of the spine. It also has to have restraints to prevent damage to itself and the other spinal structures such as the nerves and facets. These requirements create some major demands.
In appearance, the disc looks like a jelly donut. The jelly (called the nucleus) is made of sugars attached to a protein backbone called a proteoglycan. This structure allows it to act like a giant sponge. The jelly pulls in water from the body of the vertebra to create a high-pressure interior matrix (think of the jelly as the air pressure in a tire).
The outside of the donut is made up of about thirty rings of collagen, called the annulus, just like the plies of a tire. These rings are normally quite tough. Each layer of these rings alternates in angulation in their attachment to the bone of the vertebra.
The endplates of the disc separate the bone of the vertebral body from the interior of the disc. They are made of hyaline cartilage- the same cartilage that lines the hip and knee joints. This material creates a barrier to nutrients and oxygen entering and exiting the disc.
Facet Joints
In the back of the spine, the vertebrae are hooked together by paired joints called “facet joints”. These facet joints are true joints similar to a hip or shoulder joint. A true joint (or diarthrodial joint) is essentially 2 bony surfaces covered with cartilage, a Teflon type material, to reduce friction and allow the surfaces to glide with minimum resistance. The joint is surrounded by a capsule, effectively a stiff thick material that physically encloses and holds the joint together. The capsule prevents too much motion. The inside lining of this capsule are cells called the synovium that produce synovial fluid, the delicate fluid that lubricates the joint. There is a very thin layer of this within the joint itself and the joint is actually under a vacuum. The pop that you feel when you crack your knuckles or a chiropractor manipulates your back is the breaking of this vacuum. It is not deleterious and sometimes can be beneficial.
These facet joints regulate directional motion as the discs by themselves don’t have any directional stability. These joints allow you to bend forward and backwards (flexion and extension), as well as bend side to side (lateral bending.) The lower facet joints restrict rotation (twisting) more that the upper facets which as you will see later can cause some instability problems.
These facets also act as “doorstops”. They hook from the vertebra above onto the vertebra below to prevent the superior vertebra sliding forward on the lower one. This is important in the alignment of the lower two vertebra. These two segments sit on a “ski slope” pointing downhill. The entire weight of the upper body rests on the two lower vertebra causing significant pressure to force them down this slope. The structures that resist this downward slide are the facets. They act as bony blocks (or door stops) to prevent the slip. The discs by themselves offer little resistance to this forward force.
These facets can wear out and develop arthritis, just like any other joints. Bone spurs can form that press on the nearby nerves. There is a problematic condition where these doorstops break, called a spondylolysthesis. These pathological conditions will be discussed in another chapter.
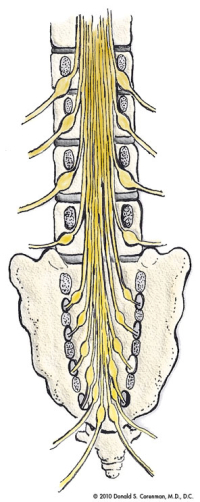
(Click to Enlarge Image) This is a cut-away front to back view of the lumbar spine which demonstrates how the nerves are distributed in the lower back. You can see which nerves are right next to the disc space and which nerves lie in the foramen (both places where the nerves can get trapped).

(Click to Enlarge Image) This is an illustration of the side view of the lumbar spine. You can see how the vertebral bodies stack up on each other and are separated by the discs in front.
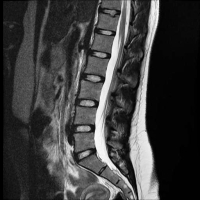
(Click to Enlarge Image) This is an MRI side view (sagittal) of the lumbar spine. Here you can see excellent disc spaces with good white signal in the discs themselves (indicates no degenerative changes), plenty of room in the canal where the spinal cord and nerves inhabit, a good curve (lumbar lordosis) and good alignment of the vertebra ( no slips or spondylolysthesis).
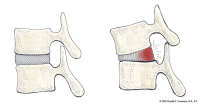
(Click to Enlarge Image) This illustration demonstrates the stresses on the back wall of the disc with standing relaxed and with flexion (bending forward). With forward bending, the back wall of the disc is stretched. With any significant load (lifting), the fibers are tensioned and can tear.
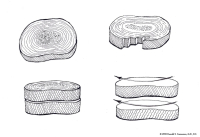
(Click to Enlarge Image) This illustration demonstrates the anatomy of the annulus. The annulus is made up of about 30 rings of collagen- just like plies of a tire. You can see that the orientation of the fibers alternate with each layer. This makes for a strong and redundant disc wall when the spine is in neutral but with twisting (rotation), half of the fibers undergo tension and the other half become relaxed. The picture on the lower right demonstrates this phenomenon. Rotation of the spine therefore weakens the disc wall and it becomes more susceptible to tearing. Moral of the story- don’t twist when you lift!

(Click to Enlarge Image) This diagram demonstrates what happens to the vertebral segments with bending forward and backwards. With forward bending, there is more compression on the front of the disc but more tension on the back of the disc. There is widening of the back of the canal including the foramen (nerve exit hole). With backwards bending, the disc has reduced pressure on it and the spinal canal and foramen are both narrowed.
