An Overview of Lumbar Foraminal Stenosis
(Collapse of the Lumbar Spine)
Lumbar foraminal stenosis (collapse of the lumbar spine) is very similar to lumbar spinal stenosis in the sense that it involves the narrowing of an area within the spinal canal. The individual nerves will exit through a small hole in the side of the spine in between the two vertebrae. This nerve root exiting occurs at every level in the spine. Do not confuse this condition with lumbar central stenosis where all the nerves in the canal are compressed. With lumbar foraminal stenosis, the compression is at the exit hole of the nerve (the foramen). Since the exiting hole is known as the foramen, narrowing of this hole is called foramenal stenosis (obviously- stenosis means narrowing). The stenosis is caused by the clogging of this nerve opening with bone spur, debris from degenerative facet disease and/or unilateral collapse of the disc (foramenal collapse).
Biomechanics
The biomechanics are very easy to understand. The nerve hole is made up of a clam shell of the vertebra above and the vertebra below. This hole enlarges with bending forward and narrows with bending backwards and to the side of the hole (right sided hole will narrow with right lateral bending). If the hole is clogged up or the nerve root is swollen (which can happen to a pinched nerve), the nerve will be compressed with standing and walking and relaxed with sitting forward, crouching and leaning over a counter (or shopping cart).
Symptoms of Lumbar Foraminal Stenosis
The most common symptom associated with collapse of the lumbar spine is unilateral or one-sided buttocks or leg pain with standing and walking. This pain goes away with sitting forward, crouching or leaning over a counter (or even a shopping cart). When the pain occurs, it normally starts in the buttocks and with prolonged standing, will radiate down the front or rear of the leg. It can be a pins and needles pain or just numbness.
Treatment of Lumbar Foraminal Stenosis
Non-Surgical
Most of the time, this lumbar foraminal stenosis is not dangerous. That is, when the nerve is compressed and pain occurs, the individual can simply lean forward to “get off the nerve”. Permanent damage to the nerve is normally less that 5%. Treatment includes physical therapy and a “flat back” program, medications and spinal injections. Education to avoid certain activities and sports that cause extension is important.
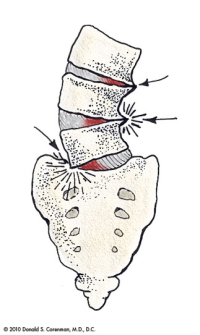
(Click to Enlarge Image) This diagram shows the angular collapse that can occur with asymmetric wear of the spine. The foramen that the nerve exits from is substantially narrowed by this collapse and nerve pain can occur with walking.

(Click to Enlarge Image) This CT scan demonstrates the narrowing of the nerve hole (foramen) from a bone spur. The arrow points to the foramen with the most significant narrowing but the one below is also narrowed by spur.
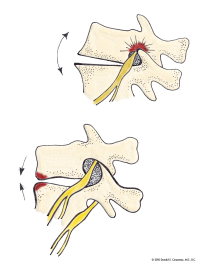
(Click to Enlarge Image) This illustration demonstrates what happens to the size of the foramen with backwards bending. The foramen becomes smaller with extension. If there is narrowing of this foramen, the nerve that exits the foramen can become compressed. Sitting and bending forward will increase the size and simply standing and walking will narrow it.
Are you suffering from symptoms of lumbar foraminal stenosis?
Would you like to consult with Dr. Corenman about your condition?
You can set up a long distance consultation to discuss your
current X-rays and/or MRIs for a clinical case review.
(Please keep reading below for more information on this condition.)
Surgical
If the compression is not associated with a collapse of the foramen, a simple microsurgical foramenotomy can be performed to treat a collapse of the lumbar spine. The recurrence rate can be as much as 10-30% depending upon the anatomy. There are cases where the vertebra is so degenerative (very little motion), a foramenectomy can be used with a better success rate. If the vertebra is collapsed unilaterally on the side of the stenosis (foraminal collapse), a TLIF (Transforaminal Lumbar Interbody Fusion) may be necessary to free the nerve and prevent future impairment to the nerve.
For more information on lumbar foraminal stenosis, or to visit with a spine specialist and back doctor in the Vail, Aspen, Denver and Grand Junction, Colorado area to discuss collapse of the lumbar spine, please contact the office of Dr. Donald Corenman.
Related Content
- When to Have Lower Back Surgery
- Causes of Lower Back Pain
- Normal Spinal Alignment
- How to Describe Your History and Symptoms of Lower Back and Leg Pain
- Best Questions to Ask When Interviewing a Spine Surgeon or Neurosurgeon
- Degenerative Spondylolisthesis
- Ganglion Cysts
- Isolated Disc Resorption-Lumbar Spine (IDR)
- Lumbar Spinal Stenosis (Central Stenosis)
