An Overview of
A posterolateral fusion (PLF) in the lumbar or thoracic spines is one of the simplest and easiest lumbar fusions to perform. Do not confuse this fusion with a PLIF (posterior lumbar interbody fusion) as the PLIF is much more complex and similar to a TLIF fusion.
What is surgically required for a posterolateral lumbar fusion is exposure of the transverse processes and facets. These structures are located close to the skin surface in the back and sides of the spine (hence the term “posterolateral”) and are not part of the spinal canal. This is the original fusion has been utilized by spine surgeons for at least 60 years with good results.
The fusion occurs when a certain set of circumstances are followed. The bone surfaces that are to be fused are exposed, cleaned of any tissue attachments and then “burred”, damaging the outer “skin” or cortex of the bone. This sets off a healing reaction.
When bone graft material is placed between two separate but “injured” bony surfaces, the bone “interprets” that a fracture has occurred. Normally, the injured cortical surface would regrow without expanding to restore its cortical “skin”. However, when bone graft is placed between two injured surfaces, the bone grows in between these surfaces. A fusion of these two vertebrae is the result.
Motion and Pedicle Screws
If motion is allowed between these two surfaces, this motion will cause disruption of bone growth, as healing bone cells require “quiet”. Motion disrupts the growing bone cells and prevents the two surfaces from joining. This is why immobilization is necessary. This is the same reason that casts are necessary for fractures of the arms or legs-to stop motion and allow for healing.
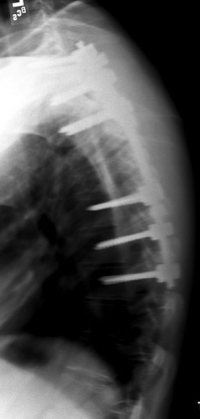
The purpose of screws and rods used in fusion is to become an “internal cast”. These implants immobilize the two bone surfaces so that bone can grow and fully join these two vertebrae together without being disrupted. The rest of the spine can still be mobile but the instrumentation will keep the individual fusion segments relatively immobile.
You might ask if the screws are still necessary after the fusion is fully solid. This hardware does become superfluous after the vertebrae become joined together. However, it is rare to have instrumentation removed after a successful fusion. These screws and rods left in place rarely cause discomfort. The hardware can be removed if necessary in a simple surgery but this occurs less than 5% of the time.
Are you a candidate for posterolateral fusion (PLF)?
Would you like to consult with Dr. Corenman about your condition?
You can set up a long distance consultation to discuss your
current X-rays and/or MRIs for a clinical case review.
(Please keep reading below for more information on this treatment.)
Indications for Posterolateral Fusion
The posterolateral fusion (PLF) may be utilized if there is no need to enter the canal and retract the nerve roots to get to the disc space.
The posterolateral fusion (PLF) does not preclude decompression such as a microdiscectomy or laminotomy to decompress the nerve roots or spinal canal. In fact, it is quite common to add one of these decompressions to the posterolateral fusion. See these decompression procedures in their respective sections on this website to understand what is involved with root decompression.
This posterolateral type of fusion is indicated in two sets of patients. Since this is a “less invasive” surgery for shorter one or two levels, those individuals who have lower demands on the lumbar spine are good candidates. An example would be an active patient with a more relaxed lifestyle who participates in golfing, biking and hiking.
The other type of individual who would benefit is the one that needs a longer fusion (more than 2 levels). Procedures like a TLIF or lateral fusion procedures for three or more levels are more complex and would require longer anesthesia times. The length of surgery risks for those fusions generally would not be beneficial to the patient.
This posterolateral fusion can however be utilized along with a more complex fusion at the base of the spine such as a TLIF to gain a longer construct with better chance of solid fusion. Longer fusions have a greater failure rate at the base of the fusion (at the sacrum, L5-S1) and a TLIF will reduce this failure rate substantially.
The most common example would be of a fusion from L1-S1 due to a degenerative scoliosis. This fusion could utilize a TLIF at L5-S1 and a posterolateral fusion at L1-L5 to create a hybrid fusion.
Another example of indications for a longer posterolateral fusion (where it would be more dangerous to involve the anterior column) is in a patient who needs a thoracolumbar fusion due to Scheuermann’s disorder or a fracture. The spinal cord generally ends at the L1 vertebra. The presence of the spinal cord in front would make an approach to this disc space more risky.
The PLF fusion can be performed with or without BMP (bone morphogenic protein). BMP tends to significantly increase the rate of fusion. See the section on BMP to understand this product.
To learn more about
Related Content
- Anterior Lumbar Interbody Fusion
- XLIF/DLIF Far lateral Interbody Fusion
- Microdiscectomy or Fusion?
- Minimally Invasive Lumbar Fusion
- Myths of Minimally Invasive Spine Surgery
- Myths of Laser Spine Surgery
- Indications for Lumbar Fusion
- X-Stop Procedure
- Artificial Disc Replacement (ADR) for Lumbar Spine
- Transforaminal Lumbar Interbody Fusion (TLIF)