An Overview of Far Lateral Lumbar Spine Fusions: Oblique Lateral Interbody Fusion (OLIF) & Extreme Lateral Interbody Fusion (XLIF)
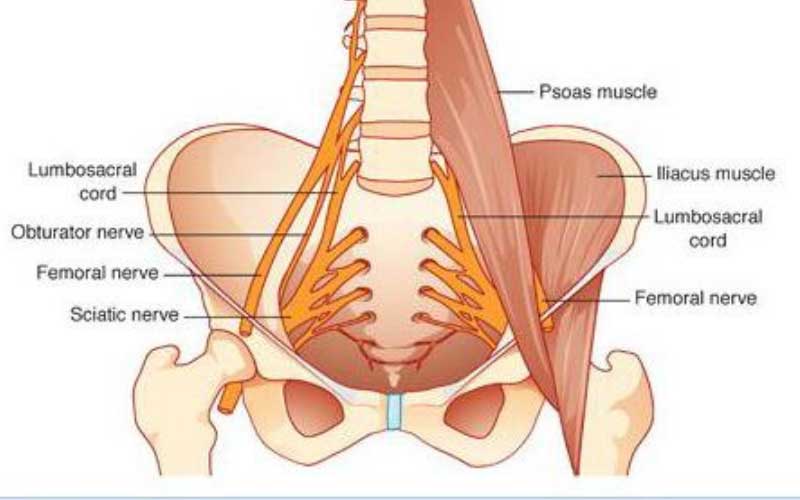
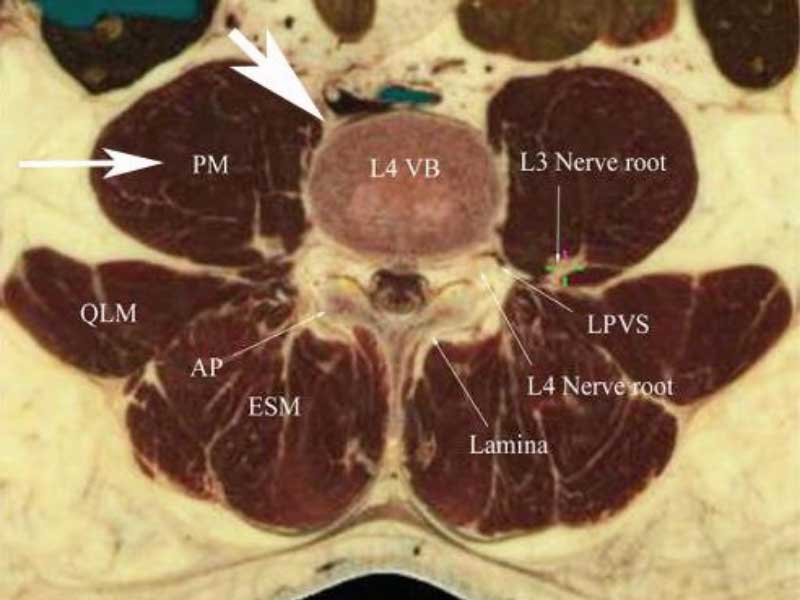
The XLIF was the first procedure to be developed to approach the vertebral body from the side which avoids the anterior approach and all the potential morbidity of going straight through the front of the belly wall. The XLIF procedures works reasonably well but does require the psoas muscle to be split (cut) to reach the side of the vertebra and the disc. The psoas muscle contains all the exiting nerve roots from L1-S1 including the femoral and sciatic nerves. These are essentially all the nerves that service both legs. These XLIF procedures required entering the muscle belly and cause retraction of the muscle containing these nerve roots which puts these nerves at risk.
The OLIF procedure was developed to prevent the need to split the psoas muscle and prevent injury to the imbedded nerve roots. This is accomplished by the “oblique” approach (the “O” in OLIF) instead of the direct lateral approach. The OLIF procedure is very good for patients with a significant deformity where one vertebra is angulated or collapsed on another and is a powerful tool to realign the spine compared to a purely posterior approach.
The approach is made through a small incision (normally 3 inches or less) on the side of the belly about where your arm would set when it hangs down from your side when standing. A small amount of abdominal wall muscle is incised and the pathway to the spine is found between the peritoneal sac (the sack containing the bowels) and the front of the psoas muscle. The psoas muscle is left fully intact but a small portion of the psoas insertion at its attachment to the vertebral body is pushed slightly back for access to the disc space. Since the important spinal nerve roots imbedded in the psoas muscle are not retracted or compressed, there is significant reduction of compression injury to these nerves (which was much more common in the XLIF approach).
This side of the disc space is opened and various “spreader tools” are used to redevelop the original disc space height. The disc is then “cleaned out” to remove cartilage and nucleus. A cage (really just a spacer) filled with bone substitutes is then inserted to hold the space open and induce fusion with its contents.
The cage is made out of PEEK (polyether ether ketone), a plastic material that is inert and non-reactive to human tissues. This cage acts as a spacer to hold the vertebra apart and in appropriate position. The cage is filled with BMP and DMP (bone morphogenic protein and demineralized bone matrix), two substances that induce new bone formation. For this part of the surgery, patient’s bone graft does not need to be taken.
XLIF or OLIF cages have to be stabilized by posterior instrumentation (pedicle screws) to make sure the cage does not “slip” out of position before the vertebra heals together. Screws can be placed by various posterior procedures.
The OLIF is designed to distract the vertebral bodies apart. This separation can indirectly reduce the compression of the neural elements in the canal or foramen but this is not guaranteed to fully free the nerve roots. This is called “indirect decompression”.
During the procedure, nerve monitoring is necessary to make sure there is no irritation or injury to the exiting nerve roots that can occur with the placement of the retractor or that too much distraction is not employed as this can on occasion cause a nerve root stretch or compression injury.
Example
These are X-rays before and after of a patient who had a long laminectomy for lower back pain that did not give him relief. This is because his pain was generated from disc degeneration and not canal narrowing (stenosis). The laminectomy makes a TLIF at all levels very difficult so OLIFs were employed at L2-3, L3-4 and L4-5 where a TLIF was utilized at L5-S1.
For more resources on