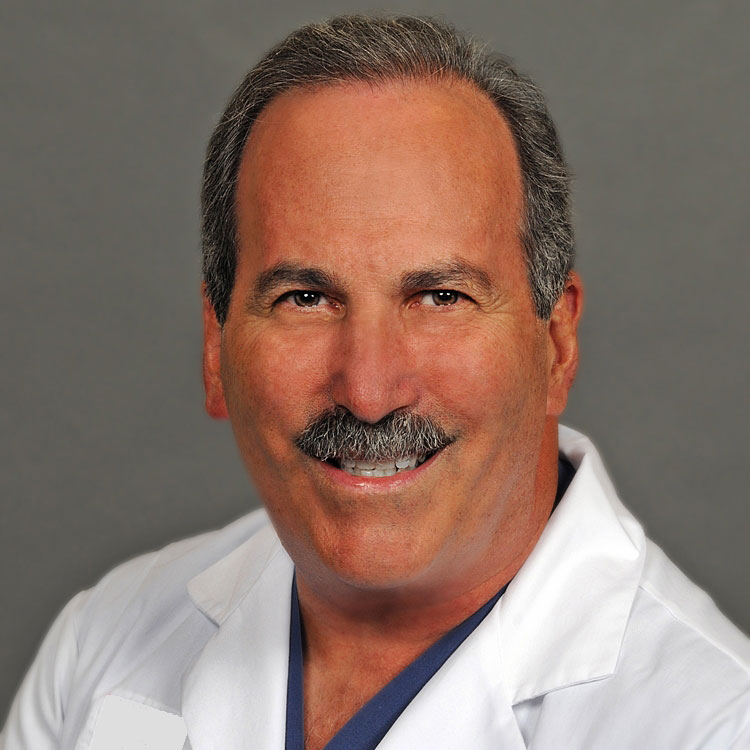
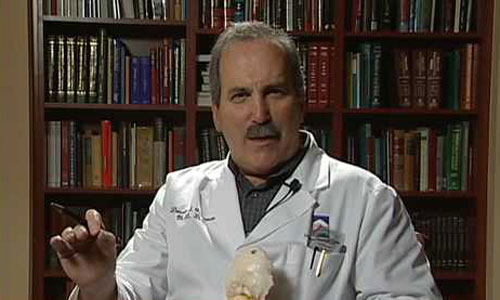
Donald Corenman, MD, DC
Spine Surgeon & Back Pain Expert
Surgical Second Opinions
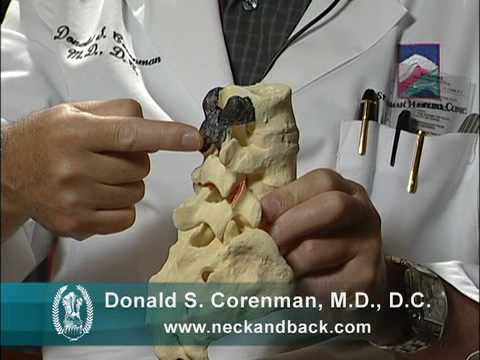
With more than 30 years of experience, Donald Corenman, MD, DC, is a highly-regarded spine surgeon, considered an expert in the area of neck and back pain. His training as a Doctor of Chiropractic early in his career did not satisfy his desire for a deep understanding of the mechanics of the spine. This led him to medical school where he completed his Doctor of Medicine, Orthopedic Surgery Residency and Spine Surgery Fellowship. His study of spinal disorders and deformities brought him to Vail, Colorado where he joined The Steadman Clinic in 1994 and practiced there until 2021. With personalized clinical care as the cornerstone of Dr. Corenman’s practice, he has been awarded the “Top 10 Doctor Award”, “Patient’s Choice Award”, “Compassionate Doctor Recognition” and is consistently recognized by Becker’s Spine Review in “Top Spine Surgeons to Know.”
Dr. Corenman has published two books: for patients, “Everything You Wanted to Know About the Back: A Consumers Guide to the Diagnosis and Treatment of Lower Back Pain” and for the medical community, “The Clinician’s Guidebook to Lumbar Spine Disorders: Diagnosis & Treatment”. He is passionate about educating patients on spine anatomy and disorders, so they have the ability to partner with their physicians in finding the most effective treatment for their back pain and disorders. His focus on peer education earned academic appointments as Clinical Assistant Professor and Assistant Professor of Orthopaedic Surgery at the University of Colorado Health Sciences Center, and his research on spine surgery and rehabilitation has resulted in the publication of multiple peer-reviewed articles.
How to Use This Website
Dear NeckandBack.com Visitors,
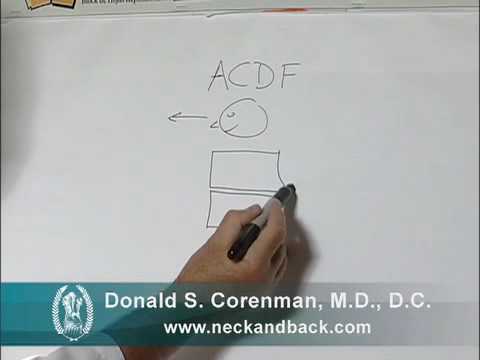
I personally created all of the content on this website to help you increase your knowledge of the spine, what can go wrong and what treatment options you have.
We start with spine anatomy and physiology (how the spine functions and why it works that way). Then we discuss spine pathology (what can go wrong and why it does). We then discuss how to diagnose what causes the spine pain and dysfunction (the pain generator or generators) and finally what to do about it (treatment for neck and back pain).
There are many options available for your treatment. Some of these have a high percentage of success and some are much less successful. When you understand what the pain stems from, the typical unfounded fears of paralysis or “being left as a cripple” leave and you can make good decisions on a sound scientific basis. You won’t normally have to ask what the recommended treatment is as this decision becomes self-evident. You should not have to ask, “What would you do if you were in my shoes?”
If you need more detailed information on your specific case, you can also ask me general questions in my forum or request an MRI review.
Sincerely,
Dr. Corenman
Spine Education Books
Everything You Wanted To Know About the Back
If you are considering physical therapy, chiropractic, medications, ergonomics, injections or even surgery as a treatment for your back pain, this is a must read!
The Clinician’s Guidebook to Lumbar Spine Disorders: Diagnosis & Treatment
An in-depth look at why back pain exists created for clinicians to offer a comprehensive understanding of lumbar spine disorders.
Professional Spine Training from Donald Corenman, MD, DC
Dr. Corenman offers the training website StudySpine.com to provide professionals who deal with spinal disorders in their daily practice with the knowledge necessary to accurately diagnose a patient’s condition and develop an appropriate treatment protocol.
His CME accredited lecture Lumbar Spine A-Z is a weekend course that covers taking a history, examination, and interpretation of MRIs and X-rays. Participants with gain the tools to understand as well as develop a differential diagnosis and treatment program for most lumbar spine disorders.