Lumbar Overview
Laminotomy means “partial removal of the lamina”. The lumbar laminotomy procedure is a “roto-rooter” job (decompression) to open a pathway for a nerve or group of nerves that are being compressed by excess bone spur, ligament or disc in the spinal canal.
The procedure has been called a lumbar laminectomy in the past. Laminectomies are generally no longer performed as there is generally no reason to remove the entire lamina. LaminECTOMY means removal of all the lamina and removing only the compressive portions of the lamina is a laminotomy (laminOTOMY-partial removal of the lamina).
These obstructions to the nerve pathway compress the nerve in certain spinal positions (typically standing and walking). Symptoms include pain, numbness, paresthesias (pins and needles) and weakness of one leg or both legs.
These symptoms occur due to stenosis, a narrowing of a nerve passage. This narrowing is related to degenerative changes in the spinal canal, which in turn compresses the canal contents.
When the disc degenerates, not only the height of the disc is affected but the facets in back then imbricate (collapse on each other). This increased pressure causes two problematic conditions.
One is the facet capsule (the bag that surrounds the facets) becomes redundant (in-folds into the canal) which causes crowding of this tunnel. The other problem is that increased pressure on these facets causes further arthritic degeneration over time.
A similar recognizable condition is hand arthritis. If you have seen older individuals with longer standing hand arthritis, you will recognize that the knuckles of their hand have enlarged and are quite bulbous. This is the same problem that occurs in the spine. These bulbous-enlarged facets (knuckles) crowd out the nerves in the canal.
Types of Stenosis
There are three types of stenosis; central stenosis, lateral recess stenosis and foraminal stenosis. Each type has a certain discrete set of symptoms. To understand each type, a description of the anatomy and biomechanics is required.
The spinal canal changes in diameter (and volume) with different positions. Flexion (bending forward) causes the canal to open up literally about 30% increase of volume. Extension (bending backwards) reduces the canal diameter by the same amount.
Standing up requires extension (bending backwards) in order to get the torso over the pelvis for balance. Walking require less extension than standing but still requires a certain amount of bending backwards to align the upper body over the pelvis. This means that further narrowing of the canal by walking and standing will cause compression to the nerve root or the entire collection of nerve roots.
Central Stenosis Laminotomy
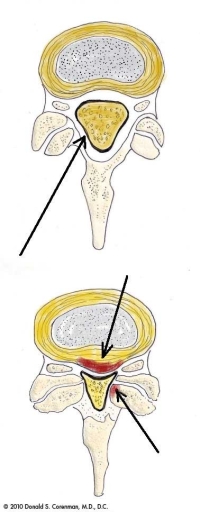
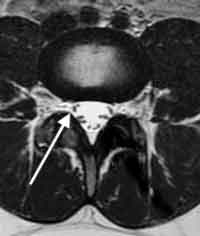
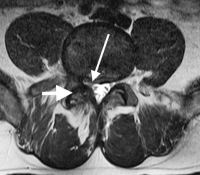
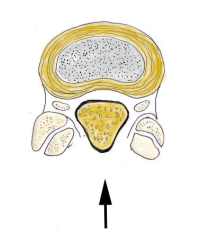
The nerves of the lower back travel through a number of tunnels. The central canal is the center tunnel that all the nerves travel in. In this tunnel, the nerves all travel in a group in a central sack called the dural sac. The nerves then branch into individual radicular nerves (nerves that have their own dural coating) while still in the central canal, like branches of an evergreen tree.
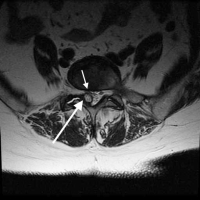
Central stenosis occurs when the main canal narrows enough to compress the entire sack of nerves. This causes a set of symptoms called neurogenic claudication (see this website for neurogenic claudication and lumbar spinal stenosis).
If there is enough narrowing due to degenerative changes (bone spurs or ligament overgrowth), these symptoms will occur when the canal narrows to a critical diameter and the nerves become too compressed.
The laminotomy procedure opens up the entire canal by removing a portion of the roof of the canal and any bone spurs and ligamentum flavum that are crowding the canal.
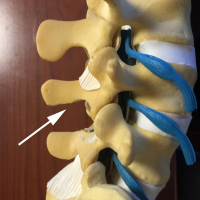
To understand how this procedure works, it is helpful to think of the spinal canal like a house with a roof. The floor of the house is made up of the disc and vertebral body. The sides are made up of the inside edges of the facets, capsules (the “wrapping” of the facets) and the ligamentum flavum (a thick vestigial elastic ligament). The roof is made up of this ligamentum flavum and the lamina (the back portion of the bone of the canal.
With stenosis or narrowing of the central canal, there are bone spurs that grow from the facet and disc edges into the spinal canal from the floor and sides. There occasionally is also a disc bulge or herniation that also crowds out the canal from the floor. From the roof, the ligamentum flavum thickens and pushes down from the top of the canal.
During the lumbar laminectomy or laminotomy procedure, to remedy this overcrowding, a portion of the lamina (the roof of the house) is removed along with the ligamentum flavum. (see illustration) Any spurs off the facets that are crowding in from the sides are also removed. If there is a disc herniation, it is removed and some disc spurs may be compressed back into the body of the vertebra. The canal is irrigated and a Valsalva maneuver is performed to make sure there is no dural leak. The incision is closed and the patient sent to recovery.
Lateral Recess Stenosis Laminotomy
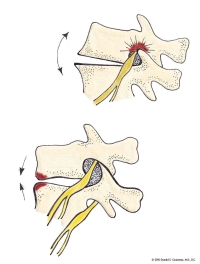
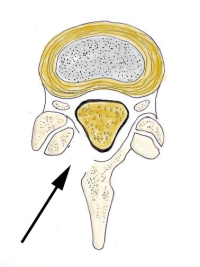
Once the nerve exits from the main sac of nerves, it travels in the lateral recess in the side of the canal. This is not a true tunnel as there is bone on three sides but not all four. It is here that this nerve can be compressed by bone spur and ligamentum hypertrophy (increased ligament bulk).
The reason this “tunnel” can be individually narrowed has to do with the location of the facet right above the nerve root. The floor of the lateral recess is the disc space, the side is the facet and the roof is the facet and ligamentum flavum. You could imagine that this nerve can be “crowded out” by degeneration of any of these structures. This in fact occurs with some frequency.
Lateral recess stenosis generally causes leg pain upon standing and walking only on one side (unilaterally). Symptoms can be increased with bending to the side of pain and decreased if bending opposite to that painful side.
The laminotomy to surgically open the lateral recess is generally only performed on the painful side. (see illustration) A small portion of the inside of the degenerative facet is removed and any ligamentum flavum that is impeding the nerve root is also removed. If there is a disc bulge or bone spur from the disc space that impedes the nerve root, that bulge is also removed.
Foraminal Stenosis Laminotomy (Foraminotomy)
The foramen is a true bony tunnel that the nerve finally exits from the spine. The foraminal tunnel consists of the pedicle above, the pedicle below, the facets as the roof and the disc wall/ vertebral body as the floor. Over half of the height of the foramen is made up by the height of the disc space.
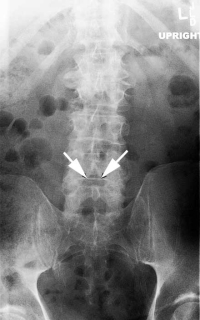
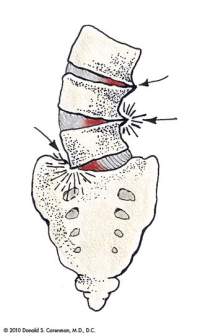
You could imagine that if the disc becomes degenerative and loses height, this would impact the size of the foramen and you would be correct. If the disc uniformly degenerates (both right and left side collapses the same amount), the foraminal stenosis will be “balanced” Depending upon the amount of collapse, a foraminotomy can be performed.
This is performed by first creating a unilateral (one-sided) laminotomy as found in lateral recess decompression. The foramen is then opened by using a curette (a scraping tool) to work around the nerve root and remove any bone or ligament impinging on the nerve.
If there is foraminal collapse due to angulation of the vertebra (see last illustration), recurrence of this narrowing can occur. The bone removed to open the foramen initially developed in that location to “shore up” this level. Removal of this bone can allow further collapse and a need for a fusion to prevent further nerve compression.
Degenerative Spondylolisthesis Association
There are times that this laminotomy procedure is performed on a level that already has a vertebral slip (see degenerative spondylolysthesis elsewhere in the web site). If the slip is not unstable (does not move much on flexion and extension x-rays) and the amount of slip is not significant, this laminectomy can be performed without stabilization (fusion). It should be noted that there are occasions that removing the spurs from the facets can lead to more slip or instability. Remember that the spurs developing off the facets formed to try and make the vertebra more stable. Removal has between a 15-30% chance of creating more slip. These numbers do not pertain to any level that has no slip.
If you live in the Vail, Aspen, Denver and Grand Junction, Colorado area and would like additional resources on lumbar