Lumbar Degenerative Disc Disease as a Cause of
Lower Back Pain
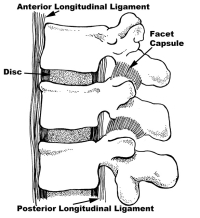
Chronic back pain and the reasons why lower back pain exists, such as lumbar degenerative disc disease (DDD), can often be explained by looking at the overall anatomy of the spine. Mechanically, everything associated with the anatomy of the lumbar spine revolves around the disc. To understand this better, it helps to gain an understanding of the function of the lumbar spine. The disc functions like a shock absorber. This structure absorbs impact and still allows for motion of the spine. It also has to have restraints to prevent damage to itself and the other spinal structures such as the nerves and facets. These requirements create some major demands. We will discuss those demands and offer causes of low back pain and reasons to why lower back problems exist.
In appearance, a disc of the lumbar spine looks like a jelly donut. The jelly (called the nucleus) is made of sugars attached to a protein backbone called a proteoglycan. This structure allows it to act like a giant sponge. The jelly pulls in water from the body of the vertebra to create a high-pressure interior matrix (think of the jelly as the air pressure in a tire).
The outside of the donut is made up of about thirty rings of collagen, called the annulus, just like the plies of a tire. These rings are normally quite tough. Each layer of these rings alternates in angulation in their attachment to the bone of the vertebra. The endplates of the disc separate the bone of the vertebral body from the interior of the disc. They are made of hyaline cartilage-the same cartilage that lines the hip and knee joints. This material creates a barrier to nutrients and oxygen entering and exiting the disc.
Common Causes of Degenerative Disc Disease
Blood Supply and Imbibition
Spine doctors are often asked to explain what is a degenerative disc and why does lower back pain exist. When someone experiences lower back pain that does not go away, they may assume they have a slipped disc, a pinched nerve in the lower back, or a compressed nerve in the spine. The problem, in reality, goes much further than this. Problems exist with the design of the disc that causes the “disease” we know today as lumbar degenerative disc disease or DDD. The first problem is that the blood supply, for all intensive purposes, disappears from the disc by about the age of eight. This means that collectively, the discs are the largest structures in the body that have no blood supply.
Without a blood supply, there is very poor oxygen penetration into the interior of the disc. The only fluids that can be exchanged are under hydrostatic and osmotic pressure. This means that motion of the disc exchanges fluids similarly to a squeezing a sponge under water and releasing it. The water and nutrients that this material absorbs and releases, transfers through the endplate of the vertebra under a process called imbibition.
The fluids that are transferred into the disc are poor in oxygen and limited in nutrients. This creates a problem for the living cells inside the disc. These cells produce the glycoproteins, which make up the nucleus, (the gel or sponge) and they need oxygen to function well. Without oxygen, these cells become much less effective keeping up with maintaining the jelly. Without the production and maintenance of these gel proteins, the pressure in the disc drops with age.
Pressure Drop
When the pressure drops inside the disc, this is similar to letting some air out of a car tire. As the pressure in the car tire drops, the sidewalls bulge outward from the weight of the car. When you then try to drive on a partially filled tire, there is less stability to hold the road, especially with unpredicted maneuvers such as a quick turn to avoid an obstacle or driving over an unexpected speed bump. Just as the car has trouble holding the road, a degenerative disc of the spine is much less resistant to abnormal movements and these motions can tear the disc wall. An injury or unexpected lift or fall may injure the disc. That is why once an individual has been diagnosed with degenerative disc disease or degenerative facet disease, proper lifting techniques become very important. Proper lifting is one of the key areas regarding how to prevent back injuries.
Annular Tears and Nociceptors
If a tear occurs, without a blood supply, the disc can’t heal if injured. One of the most common causes of low back pain is a tear. All injuries to the disc therefore are cumulative or add up. To say it another way, any injury to the disc is essentially, a permanent injury. A tear of the collagen in the donut won’t repair itself. The cells lining the outside wall of the annulus attempt to repair the outer defect but are unsuccessful and actually get in the way.
There is a tenuous blood supply in the outer 1/3 of the disc. Tears that go out to here will attempt to heal but the scar tissue laid down is not nearly as strong as the collagen fibers it attempts to replace. To make matters worse, in regards to lumbar degenerative disc disease, any blood vessels that grow into the torn fibers of the disc carry along with them new pain fibers. These fibers are highly sensitive and another major cause of pain sensitization of the disc.
The back portion of the disc (posterior annulus) is full of pain sensors called nocicepters. When a tear occurs in the annulus of the disc, these pain receptors come in contact with the nucleus of the disc. These pain receptors themselves then become inflamed and much more easily transmit pain signals.
Your Mom and Dad
The second problem with the disc (and whether you will have the symptoms associated with lumbar degenerative disc disease) is how you picked your mom and dad— genetics. This has to do with the type of collagen that makes up the plies of the tire (the annulus.) The collagen in the annulus is not uniform. Some fibers are pliable and resilient and can undergo multiple loading cycles without any wear just like thick bungee cords. Other types of collagen are unfortunately brittle, like wire coat hangers. You can bend these only a limited amount of times before they break from fatigue failure.
Good examples of this genetic relationship are the variety of patients I am asked to see. Some are injured on the ski slopes. Eighty, and occasionally, ninety years olds will sporadically develop pain in their backs and have an MRI performed through the emergency room (it helps to review another section on this website: understanding an MRI of the lumbar spine). There are times these octo and nanogenarians have perfect appearing discs. On the other end of the spectrum are the unfortunate twelve year olds in my practice with severe degenerative disc disease; while back pain in children is not too uncommon, finding severe DDD in a child does cause some alarm.
Remember Wiring!
There is a big caveat here. Remember, just because the patient may have degenerative disc disease does not mean they are going to have symptoms of lower back pain. A study out of Emory University noted that more than 60% of individuals without back or leg pain had degenerative changes in their discs. These people had no symptoms. I am always reminded of this when I see older NFL players with horrible looking spines and minimal to no pain. This leads into the theory of wiring.
There are 2 groups of patients with the same problems found on x-rays and MRI. One group has no symptoms and the other may be incapacitated with the same type of degenerative spine. It appears that some individuals are “wired” to have low back pain and others are not. This effect has to do with the sensitivity of the central nervous system and the number of pain receptors present and active in the area of injury. For example, I personally have a degenerative disc at L5-S1 and have virtually no low back pain. Others with the same type of disc on MRI are incapacitated. I have lousy wiring and am so grateful that my spine is so uneducated.

(Click to Enlarge Image) Normal midline (sagittal) MRI. Note the high signal (white) within the disc space (arrows) indicating good hydration of the nucleus. Disc space is also tall.
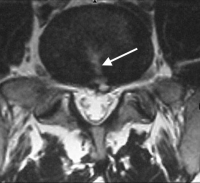
(Click to Enlarge Image 0 Axial MRI of annular tear. The white arrow points to the tear in the annulus and there is a small disc herniation at the end of the tear.

(Click to Enlarge Image) Annular tear with good disc height and hydration. Arrow points to tear of back of annulus. Note small bulge in back wall.
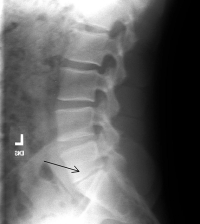
(Click to Enlarge Image) X-ray lateral of isolated disc resorption. The black arrow points to the significant narrowing of the disc space.
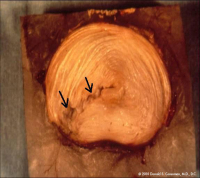
(Click to Enlarge Image) This is a laboratory specimen of a lumbar disc. The disc was loaded in torsion (twisting). Note the tear in the annulus (arrows) that was induced from the torsion. The tear goes through and through.
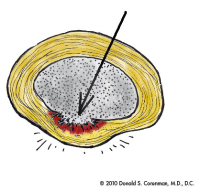
(Click to Enlarge Image) This illustration is a top down view of a degenerative bulge in the back of the disc. You can see some of the fibers are torn and others are stretched out to create the bulge.
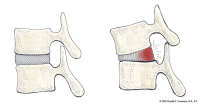
(Click to Enlarge Image) This illustration demonstrates the stresses on the back wall of the disc with standing relaxed and with flexion (bending forward). With forward bending, the back wall of the disc is stretched. With any significant load (lifting), the fibers are tensioned and can tear.

(Click to Enlarge Image) The first picture is looking down at an intact normal disc. (These pictures are of a lumbar spine disc but the cervical spine discs are almost exactly the same).The pink center is the nucleus (jelly in the donut) and the outer beige area is the annulus (donut of jelly donut fame). You can see the rings of collagen if you look carefully. Behind the disc lie the nerve roots seen in yellow. The facets in the back of the spine are seen in blue.

(Click to Enlarge Image) The second picture is of an annular tear in the back of the disc (arrow). The tear partially goes through the annulus. Note that the jelly pushes into the fibers of the annulus. The back wall of the annulus is full of pain receptors. This jelly is also neurotoxic so exposure of the pain nerves to this substance has an additional inflammation penalty.
Are you suffering from symptoms of lumbar degenerative disc disease (DDD)?
Would you like to consult with Dr. Corenman about your condition?
You can set up a long distance consultation to discuss your
current X-rays and/or MRIs for a clinical case review.
(Please keep reading below for more information on this condition.)
Symptoms of Lumbar Degenerative Disc Disease (DDD)
There are essentially 3 types of symptoms with lumbar degenerative disc disease. They all relate to the same area with significantly different presentations. Of course, lumbar degenerative disc disease can cause or be associated with many other problems such as degenerative spondylolysthesis, herniated disc, degenerative scoliosis and many others. The symptoms discussed here are strictly related to simple DDD of the lower back.
The first is “my back went out”. Patients will have “back attacks” where severe lower back pain and muscular lock up occurs. These muscle spasms of the spine can occur from a simple lift or twist associated with a “pop” in the back. Within hours to days, the back becomes progressively sorer until it “locks up”. It might take anywhere from 2-14 days for the symptoms to abate. Normally this symptom is from an annular tear, one of the plies of the tire mentioned above. Even though the symptoms are severe- this condition is not dangerous. Occasionally, the tear will go through and through the disc and a herniation can result. If that is the case, buttocks and leg pain will start 1-2 days after the “pop”. Please see the section on herniated disc of the lumbar spine for further information.
The second is chronic lower back pain that comes and goes associated with activity. This is the most common presentation of lower back pain. After years of multiple tears of the disc wall, the disc can develop pain sensitivity. Remember that the pain nerves are in the rear wall of the disc and with motion can be stretched and aggravated. This is the typical lower back pain that most people experience and represents common lower back problems among runners and individuals who are highly active in running sports.
The third condition is isolated disc resorption. This is where the disc essentially wears away and shock absorption is lost between the vertebrae. With any impact activity, the upper torso essentially bounces up and down on an inflamed bony surface of the exposed vertebral body causing stress fractures of the vertebrae. These patients have grueling pain in the back that increases with most sports activities. The very common refrain is “I’m not going to do that because I’ll pay for it later”. Many patients are incapacitated with lower back pain.
Treatment of Lumbar Degenerative Disc Disease (DDD)
Non-Surgical
The first thing to know about lumbar degenerative disc disease (DDD) and low back pain, is that it is not dangerous. Even the patients that have incapacitating lower back pain from DDD are in no danger of paralysis and won’t be in a wheel chair. The condition is like knee arthritis. Yes it is painful and yes it prevents certain activities but by itself, it is not hazardous. Degenerative disc disease can often cause arthritis of the spine, but this is often manageable with conservative therapy.
Treatment for any of the three conditions noted above is pain control, strengthening, endurance and education. Physical therapy is the mainstay. A good therapist can strengthen core muscles, teach a neutral spine program and get rid of bad habits that put the spine under more stress. A good Chiropractor that uses rehabilitation along with manipulation can be very beneficial. Cardiovascular exercise is very helpful to increase pain tolerance and strength.
Medication to help with the flair-up is very useful. Epidural injections can be wonderful for severe onset of incapacitating symptoms. Depression commonly goes along with chronic low back pain and treatment for this condition can reduce pain as well as depression.
Alternative therapies can be useful. Acupuncture seems to be helpful to control symptoms temporarily but doesn’t seem to offer “cure”. Traction is similar to acupuncture-when you get off the traction table, gravity takes over again.
Surgical
For individuals with chronic back pain and severe degeneration, surgery may be recommended. As the degeneration continues to increase, other conditions can develop such as a herniated disc or a compressed nerve in the spine–all causing significant back pain. If all non-surgical measures fail, there is spine surgery to consider. Normally, a spinal fusion surgery of the painful segment is in order. There are various tests to determine which is the painful segment. Success rate in the right patient with the right spinal fusion surgery should be close to 90% for 2/3 relief of pain.
There are various fusion surgeries to consider including a fusion from the front of the lumbar spine (anterior lumbar interbody fusion surgery, or ALIF) or fusion from the back of the spine (transforamenal lumbar interbody fusion surgery, or TLIF surgery). A lumbar laminectomy or laminotomy procedure is a roto-rooter job to open a pathway for a compressed nerve in the spine, or a group of nerves that are being compressed which can be found in patients with degenerative disc disease. Artificial disc replacement is a newer technology. In my opinion, it is useful for the neck but is not yet designed well for the lower back. This is something that can be considered for arthritis of the spine.
For more information on causes of lower back pain, such as lumbar degenerative disc disease (DDD), please contact Dr. Donald Corenman, spine specialist and back doctor offering diagnostic and surgical second opinions to patients in the USA and around the world.
Related Content
- How to Describe Your History and Symptoms of Lower Back and Leg Pain
- Best Questions to Ask When Interviewing a Spine Surgeon or Neurosurgeon
- When to Have Lower Back Surgery
- Normal Spinal Alignment
- Anatomy of Lumbar Spine
- Lumbar Spinal Stenosis (Central Stenosis)
- Chronic Radiculopathy
- Isolated Disc Resorption-Lumbar Spine (IDR)
- Lumbar Degenerative Facet Disease