Overview
Anatomy
The pelvis is made up of a ring of three bones, the two iliac wings and the sacrum, the triangular bone that is sandwiched in between them. In the front of the pelvis, the pubic symphysis attaches the ilium bones to each other. This pubic symphysis joint is very immovable due to heavy fibrous tissue joining these bones in a configuration called a syndesmosis.
In the back of the pelvis, the area where each ilium bone joins the sacrum is called the sacroiliac joint (SIJ). The sacroiliac joints are mirror image joints on each side of the sacrum.
The sacroiliac joints (SIJ) are complex in that they are made of two different types of joints combined into one. The rear portion of the joint contains both tough fibrous and ligamentous tissue regions. The front portion of the joint has aspects of regular joints like the hips and knees (called diarthrodial joints).
The rear of the SIJ binds the pelvis together. These tough fibrous bands prevent most motion. The front third of the joint is made of two opposing bony surfaces that are irregular but interdigitate together. They are covered by hyaline cartilage (the same substance that lines hips and knees) and have a thin capsule that encloses this joint. The capsule is lined with synovial tissue (the tissue that makes the lubrication for these joints).
The SIJ does not act as a typical joint like a hip or knee. There are no “gliding surfaces” like you would expect from the shoulder but a solid interlocking interface between these two bony surfaces. Unlike any other synovial joint in the body, SI joint function is designed to bond the pelvis together at the rear to make the pelvis a relatively rigid ring. This joint has about 1-2 degrees of total motion.
The SIJ changes with age. In infants, this joint surface is smooth. As we age, the peaks and valleys grow until the joint is like a jigsaw puzzle and has almost no motion. In just about everyone as we age, this joint becomes stiffer. Sometimes the joint actually fuses together. In women, the joint is somewhat looser as women must be able to deliver at the end of pregnancy. The hormone Relaxin, which loosens all ligaments in the body of women who are pregnant, also accommodates this loosening.
Sacroiliac Pathology and Chiropractic Treatment
SI Joint Pain
A controversy is whether the sacroiliac joint can actually be a pain generator. There is no doubt that the SIJ can cause pain as exemplified by the disease process called ankylosing spondylitis, an autoimmune disorder that attacks the SIJ. Patients who have ankylosing spondylitis develop inflammation of this joint demonstrable on MRI and develop true SI joint pain.
The problem with diagnosis of pain generation from the sacroiliac joint is that most pain that centers over the SIJ actually does not originate from this joint. All of the structures of the lumbar spine (disc, facet and nerve) will refer pain directly to this joint. Sacroiliac pain is really a “waste basket” of pain referral sources. Mild nerve compression will radiate down to the SIJ commonly without descending lower into the leg. Disc pain will refer into this joint and facet pain will also descend into the sacroiliac joint
As noted, nerve compression type pain from the lumbar spine (a herniated disc or other nerve compression syndrome) is the normal cause of leg pain. You would therefore think then that pain in the SIJ that radiates down the leg would rule out this joint as the source of the pain. The conundrum is that even some leg pain associated with SI joint pain can originate from the SIJ.
The sciatic nerve sits in front of the sacroiliac joint and can become irritated by a tear in the anterior capsule of this joint. Injury to this capsule can cause secondary inflammation of the sciatic nerve with resultant leg pain. This means in rare circumstances that the SIJ can cause leg pain. It is just rare.
This brings me to reinforce the point that pain in the SI joint is almost never generated from the joint itself. In fact, the chance of sacroiliac joint region pain originating from the joint is about 1%. Nonetheless, this joint can cause pain in certain circumstances.
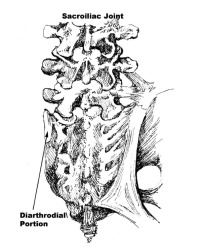
(Click to Enlarge Image) This is a back to front picture of the sacroiliac joint. The left side demonstrates the diarthodial portion (lined with cartilage) and the right side with the tough ligamentous portion.
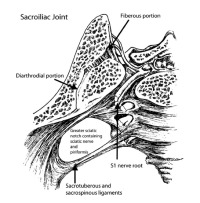
(Click to Enlarge Image) Top-down image of the sacroiliac joint. To the right is the sacrum and left is the ilium. You can see both portions of the joint (the diarthodial portion that is like the hip or knee joint and the fibrous portion which is stiff and unyielding.
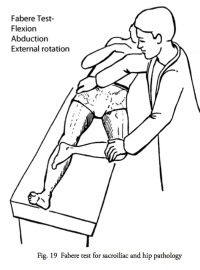
(Click to Enlarge Image) This FABERE test (flexion, abduction, external rotation) is sensitive for sacroiliac syndrome but is commonly positive in many other disorders.
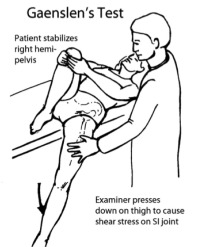
(Click to Enlarge Image) The Gaenslens test is probably the most sensitive test for Sacroiliac syndrome but is commonly positive in other disorders.
Diagnosis of
Diagnosis of is difficult in that there are very few physical examination tests that can insure a diagnosis of SIJ syndrome. These include the Patrick’s FABERE test, the Gaenslen’s Test, the pelvic compression test and the pelvic shear test. These tests will be positive in most patients with SIJ syndrome but will also be positive in other spinal conditions. Direct palpation of this joint with resultant tenderness is not helpful for diagnosis.
X-rays are also generally not helpful for diagnosis of . Many individuals have degeneration of the SIJ based upon X-rays and have absolutely no symptoms. Others with obvious SI joint pain from the joint itself have normal looking joints on X-ray. MRI scans can be more helpful for significant bone changes indicating abnormal loading and wear.
MRI is the gold standard for diagnosing ankylosing spondylitis and the seronegative spondyloarthopathies. MRI might be somewhat more helpful in diagnosing SIJ syndrome but commonly will also be negative (look normal).
Diagnostic Blocks
It makes sense that using an SIJ injection with an anesthetic (Novocain, Lidocaine, Marcaine) should numb the joint and temporarily rid the patient of pain with an SIJ disorder. This is called a diagnostic block and is the mainstay for diagnosis of this disorder. The injection into the joint is normally accompanied by a corticosteroid, which can be effective for long-term relief and possibly a cure.
There is however, occasionally a problem with this diagnostic test. SI joint injections can inadvertently anesthetize the sciatic nerve if there is a joint capsule tear of the anterior joint. The sciatic nerve sits directly in front of this joint. With a tear of this joint capsule, injected fluid can leak out in front and contact this nerve.
If the sciatic nerve is contributing to SIJ regional pain (from a herniated disc for example), pain will improve from the SIJ injection but the wrong conclusion might be drawn. The doctor might think pain relief indicates an SIJ syndrome when in fact the pain is originating from the anesthetized L5 nerve root (called a false positive test).
Injection of an X-ray dye agent into the joint can reveal this tear. The dye will leak out the front of the joint and will be visible on fluoroscopy. This leak would allow the injectionist to note the tear and allow more information to be available to the diagnostician.
Treatment of
Manual Therapy
The first treatment for any suspected is physical therapy or Chiropractic manipulation. With appropriate treatment, many patients will obtain relief. Many patients will respond to this therapy. Patients who do not respond then move on to the next series of treatments. These are rhizotomies or prolotherapy.
Rhizotomies
Rhizotomy is the ablation (destruction) of the small sensory nerves that feed the sacroiliac joint to make the joint non-painful. This is performed in an out-patient setting using a small needle with a tip that heats up to create a “burn zone” for this sensory nerve ablation.
If you look at the sacrum, you will see two parallel rows of holes on the front and the back. The innervation (nerve supply) to the sacroiliac joint goes through the medial nerve branches from these back and front “holes”. In other words, these holes are where the nerves exit to enter the joint.
This location of these holes is important if you want to denervate this joint (stop the pain nerves from continuing to signal pain). Rhizotomies or destruction of the sensory nerves can only be performed on the nerves in back of the sacrum, as the anterior nerves cannot be reached using this method. This means that rhizotomies might not be 100% effective for full relief of SIJ pain. Nonetheless, this is a valuable treatment for sacroiliac pain syndrome.
Prolotherapy
Prolotherapy means “proliferative therapy”. The theory for this treatment is that injection of an irritating substance into the joint will cause tissue destruction and scar formation. Since motion tends to be the major cause of SIJ syndrome, injection of a prolotherapy substance will cause scar tissue to form in the joint and the joint to stiffen. In addition, this injection will also destroy the nociceptors (pain nerve endings) in the joint.
A tear of the anterior capsule is important to be aware of with this treatment. Prolotherapy fluid can leak out of this anterior tear and the destructive agent can irritate or even damage the sciatic nerve.
Surgery
Fusion of the SI joint is the endpoint treatment for chronic SI pain syndrome. There are some newer techniques that have been recently developed. The long-term success rate for SI joint fusion appears to be in the range of 70%.
If the patient has had a prior fusion to the pelvis with screws that cross the sacroiliac joint, removal of these screws can relieve SIJ pain and fusion of this joint may not be necessary.
For more resources on
Related Content
- When to Have Lower Back Surgery
- Causes of Lower Back Pain
- Normal Spinal Alignment
- Lumbar Spine Anatomy
- How to Describe Your History and Symptoms of Lower Back and Leg Pain
- Best Questions to Ask When Interviewing a Spine Surgeon or Neurosurgeon
- Degenerative Spondylolisthesis
- Isolated Disc Resorption-Lumbar Spine (IDR)
- Lumbar Spinal Stenosis (Central Stenosis)
