An Overview of Tarsal Tunnel Syndrome
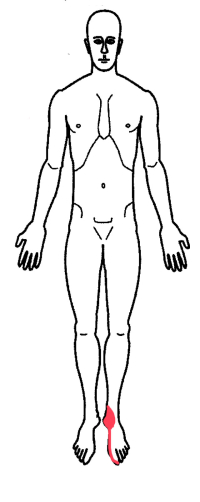
Tarsal tunnel syndrome, often referred to as tibial nerve entrapment, is a painful foot condition noted when the tibial nerve becomes trapped in the tarsal tunnel. The tarsal tunnel is named for the bones of the foot, the tarsal bones (as compared to the carpel bones of carpel tunnel syndrome found in the hand).
The tarsal tunnel is found on the inside of the ankle behind the medial malleolus (the bony bump on the inside of the ankle where the top of the shoe rests against this bone). There is a groove in the back of this bone that this nerve sits in. The outside of the tunnel is bound by a retinaculum. A retinaculum is a ligament, a thick band of non-stretchable tissue needed to hold the contents of the tunnel in place.
The tibial nerve is not alone in this tunnel. There is an artery (the tibial artery) and three tendons connected to the foot and the muscles of the lower leg that also run through this tunnel.
The tibial nerve splits into three separate nerves in the tarsal tunnel. These nerves travel to the heel and the bottom of the inside and the outside of the foot.
General Causes of Nerve Entrapment Syndromes
Most nerve entrapment syndromes are caused by mechanical and genetic problems. Genetics have to do with the size of the tunnel these nerves travel in. Some people have congenitally smaller tunnels and with aging, previous injury, degeneration (bone spurs) and inflammation, these tunnels become overcrowded. Mechanically, overuse syndrome can cause tendons to swell (tendonitis and synovitis) and crowd out the nerve.
There are genetic and metabolic disease processes that can contribute to nerve malfunction. These processes may increase the swelling (crowding) of the tunnel or make the nerve itself more sensitive. These disorders include rheumatoid arthritis, hypothyroidism, pregnancy, diabetes, acromegaly (too much human growth hormone) and CMT syndrome (Charcot Marie Tooth syndrome-a genetic condition).
Are you suffering from symptoms of Tarsal Tunnel Syndrome?
Would you like to consult with Dr. Corenman about your condition?
You can set up a long distance consultation to discuss your
current X-rays and/or MRIs for a clinical case review.
(Please keep reading below for more information on this condition.)
Symptoms of Tarsal Tunnel Syndrome
Tarsal tunnel syndrome symptoms include paresthesias (pins and needles) as well as pain radiating around the ankle and to the underside of the toes. Numbness and burning sensations can also be noted in this distribution. Standing will increase the symptoms and elevating the foot will reduce the symptoms.
Increasing nerve involvement can produce hot or cold sensations and electrical discharge symptoms (Tinel’s sign). Prolonged standing in any individual can increase the swelling of the foot in general and this swelling can worsen the symptoms of tibial nerve entrapment.
The tibial nerve moves in the tarsal tunnel with ankle motion. Plantar flexion (pushing the foot and toes to the floor) loosens the nerve and dorsiflexion (pulling the toes and foot to the nose) will stretch the nerve. Stretching the nerve will increase symptoms.
Diagnosis of Tarsal Tunnel Syndrome
History, examination and special testing confirm the diagnosis of this condition. The history is exactly like that noted above.
Testing essentially consists of one or two tests. The Tinel’s test has to do with the exquisite sensitivity of any nerve at an injury point. A nerve that is injured will fire an ectopic focus (a lightening bolt of electricity) down to the end of nerve when stimulated. Percussion of the injury area will elicit this “lightening bolt”. In the case of tarsal tunnel syndrome, the injury point is where the nerve wraps around the ankle. A positive test will cause an electrical “zap” into the foot with percussion of the nerve at the ankle.
Some physicians will perform a two-point discrimination test. This test uses the ends of monofilament fishing line on a tool that can separate these two points at a specific distance. This tool is used to determine the smallest distance that a patient can identify the distance between these two points. In tarsal tunnel syndrome, this distance will be larger than normal in bottom of the foot as the sensitivity of the skin here diminishes.
Finally, an electrical test called an EMG/NCV can be used to determine if there is conduction loss or muscle weakness. A negative test (no findings) would not preclude a diagnosis of tarsal tunnel syndrome.
Treatment of Tarsal Tunnel Syndrome
Treatment for tarsal tunnel syndrome depends upon the severity of the symptoms. Intermittent symptoms that do not bother the patient and do not wake them up at night generally do not need to be treated.
With increasing symptoms, medications such as NSAIDs (Motrin, Aleve) can be helpful. Injection of steroid into the tarsal tunnel can be effective to reduce symptoms.
If symptoms continue without relief or motor weakness occurs, surgical decompression of the nerve can provide long-term relief.
For additional resources on tarsal tunnel syndrome, or to determine treatment options for your case of tibial nerve entrapment, please contact Dr. Donald Corenman, back doctor and spine specialist offering diagnostic and surgical second opinions to patients in the USA and around the world.