Carpal Tunnel Syndrome Overview
Carpal tunnel syndrome involves trapping of a peripheral nerve in a tunnel. These peripheral nerves are different from the nerves in the spinal canal (the radicular nerves) due to their “protective armor”, the epineurium and perineurium. This protective sheath makes the nerve less vulnerable to injury than the spinal nerves. Nonetheless, these nerves can be injured by stretch, impact and compression.
You can read about the specifics of what causes the microscopic damage to a nerve in the separate topic “Nerve Injuries and Recovery” on this website.
Sensory Symptoms
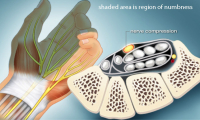
The nerve becomes compressed and then can become injured. As pressure increases on the nerve, the blood flow decreases. This causes nerve malfunction such as conduction loss and unintended conduction called ectopic stimuli. Loss of conduction means the nerve will not convey messages to the brain from the skin. This loss of sensation is obviously described as “numbness”.
Injury can also cause conduction to occur even when the nerve is not stimulated (ectopic stimulation). This is like a short circuit in doorbell wiring making the doorbell ring when no one is at the door. This sensation is noted by the patient as pain, paresthesias (pins and needles) as well as bizarre sensations (ants crawling or cold water splashing on the skin).
The continued crush injury can also injure the myelin sheath, the “insulation” of the nerve. This can be more of a permanent injury. Myelin sheath injuries can heal but this healing takes between 8-14 weeks for recovery.
With compression of the nerve, increased “pins and needles” (paresthesias) typically occur. Electric shock sensations (Tinel’s sign) that “zing” down the nerve then can occur. Abnormal spontaneous hot and cold sensations can develop in the distribution of the nerve
With chronic injury, fluid collects in the space that the nerve occupies and the nerve itself can swell, increasing the intensity of the symptoms. Continued nerve injury produces increased swelling and can induce pain. Burning sensation can occur when the nerve develops permanent injury. The pain can worsen and spread. Pain tends to be worse with activity and is relieved by rest but continuous pain can occur with chronic injury.
Motor Symptoms
For those nerves that contain motor fibers, motor strength loss typically occurs gradually. There are rare circumstances however where the entire muscle group can fail all at once. For instance, in the leg with peroneal neuropathy, this might manifest as foot drop, the inability to hold the foot up when walking. With foot drop, the foot will slap on the ground or even “catch”: the ground when the foot swings through when walking. In the case of carpel tunnel syndrome, grasp can become difficult with the effect of the feeling of clumsiness (inadvertently dropping objects).
As small muscles lose their nerve supply they can create a “cramping feeling”. Cramping can be an indication of weakness but other non-related disorders can also cause cramping.
Causes of Nerve Entrapment Syndromes
Most entrapment syndromes are caused by mechanical and genetic problems. Genetics have to do with the size of the tunnel these nerves travel in. Some people have congenitally smaller tunnels and with aging, previous injury, degeneration (bone spurs) and inflammation, these tunnels become crowded. Mechanically, overuse syndrome can cause tendons to swell (tendonitis and synovitis) and crowd out the nerve.
There are genetic and metabolic disease processes that can contribute to nerve malfunction. These processes may increase the swelling (crowding) of the tunnel or make the nerve itself more sensitive. These disorders include rheumatoid arthritis, hypothyroidism, pregnancy, diabetes, acromegaly (too much human growth hormone) and CMT syndrome (Charcot Marie Tooth syndrome-a genetic condition).
Are you suffering from symptoms of Carpal Tunnel Syndrome?
Would you like to consult with Dr. Corenman about your condition?
You can set up a long distance consultation to discuss your
current X-rays and/or MRIs for a clinical case review.
(Please keep reading below for more information on this condition.)
What is Carpal Tunnel Syndrome?
The symptoms of carpal tunnel syndrome are the most common peripheral nerve entrapment symptoms that develop in humans. Women are three times as likely to develop carpal tunnel syndrome than men, possibly because the carpal tunnel is smaller in women than in men. Individuals who work with repetitive motions of their hands are more likely to develop carpal tunnel syndrome.
Anatomy
The median nerve is the nerve that passes through the carpal tunnel. This nerve derives from the nerves of the neck (cervical nerve roots) and descends through the arm to supply the hand with motor and sensory fibers. This nerve is not alone in the carpal tunnel and its roommates are what cause this nerve to become compressed.
Carpal tunnel syndrome is caused by entrapment of the nerve as it passes through the carpal tunnel in the hand. The carpal tunnel is so named as this tunnel is made up on three sides by the carpal bones of the wrist. The carpal ligament, a tough, non-stretchy material similar to burlap or tough nylon, makes up the top boarder of this tunnel.
The carpal tunnel contains not only the median nerve but also the tendons of the fingers. Tendons are the cables that attach from the muscles in the forearm and run down to attach to the fingertips. If these muscles were located by evolution in the hand, the hand would be too big to grasp anything. These tendons transmit the power from the muscles of the forearm to the fingers and generate the grip strength.
Tendons can swell if they are irritated or overused. This would not be a problem in a large space like the forearm but in the wrist, this swelling can overcrowd the carpal tunnel and compress the median nerve.
Carpal Tunnel Syndrome Symptoms
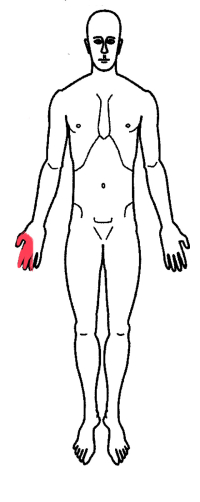
The median nerve in the hand supplies sensation to the palm side of the thumb and the first three fingers next to the thumb (index, long and one half of the ring finger). The palm itself is not generally affected by carpal tunnel syndrome as the small sensory branch to the palm exits before going through the carpal tunnel.
The median nerve also supplies motor fibers to the thumb muscles that allow the thumb to abduct or move away from the hand (hitch-hiking).
The volume of the carpal tunnel is changed by wrist position. Flexion of the wrist (bending the wrist to the palm side) will reduce the size of the carpal tunnel and extension (bending away from the palm) will enlarge it. This is why carpal tunnel syndrome will awaken some individuals from a dead sleep. Many people tend to sleep with their wrists cocked (flexed) next to their face. This position will compress the median nerve, worsen the hand numbness and will awaken these individuals in the middle of the night.
Carpal tunnel syndrome symptoms are characterized by intermittent numbness of the thumb and first three fingers. These symptoms typically occur at night or with prolonged use of the hand. If the syndrome continues, weakness of grip and a “dead” feeling of the hand can develop. The hand will occasionally need to be “shaken out” to restore this lost feeling.
If the compression continues, pain and weakness can occur in the hand on the thumb side. Grip strength can become then become compromised. Fine motor skills in this hand then can suffer. The patient might feel like they cannot hold an object without dropping it.
Carpal Tunnel Syndrome Diagnosis
History, examination and special testing confirm the diagnosis of this condition. The history is exactly like that noted above.
Testing essentially consists of two or three tests performed by a physician. Phalen’s test involves holding the wrist in extreme flexion for about 30 seconds to a minute. If carpal tunnel syndrome is present, this position will compress the median nerve and the typical symptoms are reproduced.
The Tinel’s test has to do with the exquisite sensitivity of any nerve at an injury point. A nerve that is injured will fire an ectopic focus (a lightening bolt of electricity) down to the end of nerve when stimulated. Percussion of the injury area will elicit this lightening bolt. In the case of carpal tunnel syndrome, the injury point is in the carpal tunnel where the nerve has been compressed. A positive test will “zap” the thumb and possibly the fingers with percussion of the nerve at the wrist.
Some physicians will perform a two-point discrimination test. This test uses the ends of a light monofilament fishing line on a tool that can separate these two points at a specific distance. This tool is used to determine the smallest distance that a patient can identify the distance between these two points without looking. In carpal tunnel syndrome, this distance will be larger than normal as the sensitivity of the skin diminishes, especially if compared to the opposite side.
Finally, an electrical test called an EMG/NCV can be used to determine if there is conduction loss or muscle weakness.
Carpal Tunnel Syndrome Treatment
Treatment depends upon the severity of the symptoms. Intermittent symptoms that do not bother the patient and do not wake them up at night generally do not need to be treated.
With increasing symptoms, medications such as NSAIDs (Motrin, Aleve) can be helpful. A wrist splint (called a cock-up splint) can be worn at night for symptoms that wake the patient up and can be worn full time for more severe symptoms.
Steroid injections can be placed in the carpal tunnel to reduce swelling. If symptoms continue without relief or motor weakness occurs, surgical release of the carpal ligament can provide long term relief (carpal tunnel release).
For additional resources on carpal tunnel syndrome, please contact the practice of Dr. Donald Corenman, neck doctor and spine specialist offering diagnostic and surgical second opinions to patients in the USA and around the world.
Related Content
- Carpel Tunnel Syndrome
- Cubital Tunnel Syndrome
- Thoracic Outlet Syndrome
- Nerve Entrapment/Compression
- Nerve Damage & Healing
- Normal Spinal Alignment
- Anatomy of Thoracic Spine
- Anatomy of Lumbar Spine
- When to Have Lower Back Surgery
- When to Have Neck Surgery
- How to Describe Your History and Symptoms of Lower Back and Leg Pain
- Walking (gait) Disorders