Cubital Tunnel Syndrome Overview
Cubital tunnel syndrome involves the trapping of a peripheral nerve in a tunnel. These peripheral nerves are different from the nerves in the spinal canal (the radicular nerves) due to their “protective armor”, the epineurium and perineurium. This protective sheath makes the nerve less vulnerable to injury than the spinal nerves. Nonetheless, these nerves can be injured by stretch, impact and compression.
You can read about the specifics of what causes the microscopic damage to a nerve in the separate topic “Nerve Injuries and Recovery” on this website.
Sensory Symptoms
The nerve becomes compressed. As pressure increases on the nerve, the blood flow decreases. This causes nerve malfunction such as conduction loss and unintended conduction called ectopic stimuli. Loss of conduction means the nerve will not convey messages to the brain from the skin. This loss of sensation is obviously described as “numbness”.
Injury can also cause conduction to occur even when the nerve is not stimulated. This is like a short circuit in doorbell wiring making the doorbell ring when no one is at the door. The patient will note this sensation as pain, paresthesias (pins and needles) as well as bizarre sensations (ants crawling or cold water splashing on the skin).
The continued crush injury can also injure the myelin sheath, the “insulation” of the nerve. This can be more of a permanent injury. Myelin sheath injuries can heal but this healing takes between 8-14 weeks for recovery.
With compression of the nerve, increased “pins and needles” (paresthesias) typically occur. Electric shock sensations (Tinel’s sign) that “zing” down the nerve then can occur. Abnormal spontaneous hot and cold sensations can develop in the distribution of the nerve
With chronic injury, fluid collects in the space that the nerve occupies and the nerve itself can swell, increasing the intensity of the symptoms. Continued nerve injury can induce pain. Burning sensations can occur when the nerve develops permanent injury. The pain can worsen and spread. Pain tends to be worse with activity and is relieved by rest but continuous pain and hypersensitivity can occur with chronic injury.
Motor Symptoms
For the ulnar nerve, motor strength loss typically occurs gradually. There are rare circumstances however where the entire muscle group can fail all at once. For instance, in the leg with peroneal neuropathy, this might manifest as foot drop, the inability to hold the foot up when walking. With foot drop, the foot will slap on the ground or even “catch”: the ground when the foot swings through when walking. In the case of cubital tunnel syndrome, grasp can become difficult with the effect of the feeling of clumsiness (inadvertently dropping objects).
As small muscles lose their nerve supply they can create a “cramping feeling”. Cramping can be an indication of weakness but other non-related disorders can also cause cramping.
Causes of Nerve Entrapment Syndromes
Most nerve entrapment syndromes are caused by mechanical and genetic problems. Genetics have to do with the size of the tunnel these nerves travel in. Some people have congenitally smaller tunnels and with aging, previous injury, degeneration (bone spurs) and inflammation, these tunnels become overcrowded. Mechanically, overuse syndrome can cause tendons to swell (tendonitis and synovitis) and crowd out the nerve.
There are genetic and metabolic disease processes that can contribute to nerve malfunction. These processes may increase the swelling (crowding) of the tunnel or make the nerve itself more sensitive. These disorders include rheumatoid arthritis, hypothyroidism, pregnancy, diabetes, acromegaly (too much human growth hormone) and CMT syndrome (Charcot Marie Tooth syndrome-a genetic condition).
Are you suffering from symptoms of Cubital Tunnel Syndrome?
Would you like to consult with Dr. Corenman about your condition?
You can set up a long distance consultation to discuss your
current X-rays and/or MRIs for a clinical case review.
(Please keep reading below for more information on this condition.)
What is Cubital Tunnel Syndrome?
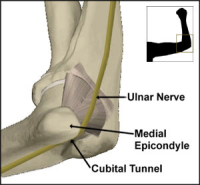
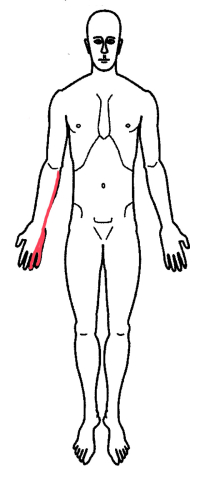
The ulnar nerve is the nerve that passes through the cubital tunnel. This nerve is also known as the “funny bone” nerve. The ulnar nerve is derived from the nerves in the neck (cervical nerve roots) and descends through the arm to supply the hand with motor and sensory fibers. The ulnar nerve is the only structure within the cubital tunnel.
The cubital tunnel is made up by the bone on the inner portion of the elbow (the medial epicondyle), which has a groove or trough in it. The ulnar nerve physically is a structure about one half the diameter of your little finger. This nerve sits in the trough (the ulnar groove) and acts like a cable in a pulley. The nerve literally moves back and forth in this trough when you flex and extend your elbow. There is almost no padding between this nerve and the skin.
If this nerve is damaged, the entire nerve can swell or the nerve can develop a small bump within the body of the nerve. Since this nerve acts like a cable in a pulley when the elbow is flexed and extended, this bump within the nerve can catch in the pulley and cause a click, which can be painful.
Continuous flexion (bending) of the elbow will stretch the ulnar nerve. With cubital tunnel syndrome, this stretching will cause symptoms to occur. Since some individuals sleep with their elbow bent, increased symptoms can awaken these individuals.
The nerve can be compressed and injured when the individual puts pressure on the elbow. This typically occurs while leaning on an armrest or resting the elbow on a counter. Occasionally, this pressure can be damaging. There is a condition called “Saturday Night Palsy” where an inebriated (drunk) individual will pass out while resting their elbow on a bar. Since the patient is unconscious her or she will not realize the pain from this nerve compression, Continued pressure will severely injure the ulnar nerve.
Cubital Tunnel Syndrome Symptoms
This nerve supplies sensation to the side of the hand opposite the thumb. This includes the small finger and the side of the ring finger. This region of the hand will develop numbness and paresthesias (pins and needles) especially if the elbow is flexed (bent) or the elbow is struck on the “funny bone”. If symptoms are severe, the numbness can wake the patient up from a dead sleep.
The median nerve also supplies motor fibers to the muscles of the hypothenar region (the outside or pinky side of the palm) and the third and forth lumbrical muscles (muscles in between the fingers). A significant injury to this nerve here would produce a “claw hand” (little and ring fingers that would be curled).
Diagnosis of Cubital Tunnel Syndrome
History, examination and special testing confirm the diagnosis of this condition. The history is exactly like that noted above.
Testing essentially consists of one or two tests. The stretch test involves holding the elbow in extreme flexion for about 30 seconds to a minute. This position stretches the ulnar nerve and typical symptoms can be reproduced.
The Tinel’s test has to do with the exquisite sensitivity of any nerve at an injury point. A nerve that is injured will fire an ectopic focus (a lightening bolt of electricity) down to the end of nerve when stimulated. Percussion of the injury area will elicit this “lightening bolt”. In the case of cubital tunnel syndrome, the injury point is in this cubital tunnel where the nerve has been compressed. A positive test will produce an electrical “zap” into the ring and pinky fingers with percussion of the nerve at the elbow.
Some physicians will perform a two-point discrimination test. This test uses the ends of monofilament fishing line on a tool that can separate these two points at a specific distance. This tool is used to determine the smallest distance that a patient can identify the distance between these two points. In cubital tunnel syndrome, this distance will be larger than normal in the ring and small fingers as the sensitivity of the skin here diminishes.
Finally, an electrical test called an EMG/NCV can be used to determine if there is conduction loss or muscle weakness. A negative test (no findings) would not preclude a diagnosis of cubital tunnel syndrome.
Cubital Tunnel Syndrome Treatment
Treatment depends upon the severity of the symptoms. Intermittent symptoms that do not bother the patient and do not wake them up at night generally do not need to be treated. Occasionally, a soft elbow pad can be used to protect the nerve from compression.
With increasing symptoms, medications such as NSAIDs (Motrin, Aleve) can be helpful. An elbow splint or even a towel loosely wrapped around the elbow can be worn at night to keep the elbow from bending and prevent the symptoms that awaken the patient.
Steroids can be injected in the cubital tunnel to reduce swelling. If symptoms continue without relief or motor weakness occurs, surgical decompression of the nerve can provide long-term relief. Occasionally, the nerve needs to be moved out of its groove and placed within the muscle of the elbow (ulnar nerve transposition).
For more resources on cubital tunnel syndrome, or to learn more about other nerve entrapment syndromes, contact the Vail, Aspen, Denver and Grand Junction, Colorado area office of back doctor and spine specialist Dr. Donald Corenman.