An Overview of Causes of Lower Back Pain
Pain in the lower back has a multitude of causes. The discs, facets, pars interarticularis, sacroiliac joints, hip joints and nerves can all be causes of lower back pain. Even compression fractures at T12 and a high grade thoracic hyperkyphosis (increased thoracic curve) can cause lower back pain. The trick is to discover what structures are causing this pain and formulate a treatment plan. Although the structures of the lower back cause the vast majority of lower back pain, this section does not take into consideration that lower back pain can also be caused by referral pain from structures not in the lumbar spine.
Commonly, patients will throw all lower back pain symptoms into the “garbage bin” of “low back pain”. When asked, “where does it hurt” many will state, “in my lower back” but not having really thought where the symptoms specifically are located.
If carefully analyzed, most of this “lower back pain” will be found to have specific locations with certain activities and that differential can make a great difference in the diagnosis of the origin of the pain. Patients will use the term “hip pain” and confusingly point to their sacroiliac joint. Patients with “lower back pain” will point to their buttocks as the center of their pain. Even physicians who come to the office with lower back pain can be confused as to the location of their lower back pain. When asked carefully directed questions as to where the pain originates, they commonly change their opinion of where the epicenter of the pain is located.
Diagnosing Causes of Lower Back Pain
The first step in diagnosis is to determine really where the pain is centered, where the pain radiates and what activities cause increased or diminished pain. I like to use the 100% rule. That is, if the total global pain picture would add up to 100%, how would you divide up the pain? Is there pain in the central lower back, pain that is most intense in the sacroiliac joint or pain that radiates into the back of the thigh or the groin? Each of these subtleties can mean a very different origin of the pain.
Pain Diagram
This is one of the most useful tools the spine expert has in diagnosing causes of lower back pain. This diagram is filled out by the patient and requires the patient to really think about the location of the epicenter of the pain and where the pain radiates. Unfortunately, this diagram will not stand by itself, as more information is needed such as what activities create and relieve the pain and what the intensity of the pain is with those activities. That is left to the visual acuity scale (VAS) and a good history (the actual questioning of the patient) by a skilled examiner.
Lower Back Pain Generated by the Disc
Lower back pain generated from disc disorders can typically occur from tears in the annulus (the outer part of the jelly-filled donut). Tears in the disc wall or annular tears typically cause the commonly heard complaint “my back went out”. New annular tears can cause severe pain, lower back muscle weakness from pain inhibition and the inability to stand upright. Interestingly, many individuals will develop these tears and have no lower back pain while some patients are incapacitated. The answer to this question deals with genetics and neurological innervation, which is not covered here.
Most times after an acute tear, the pain diminishes and the patient returns to “normal”. The tear does not heal but the pain fibers become quiescent and there are typically no further symptoms. There is however a subset of patients that will not recover and have continued pain leading to chronic lower back pain. These patients undergo therapy, injections and medications and many then recover. The ones that continue with symptoms after 4-6 months of failed care may develop chronic discogenic lower back pain or lower back pain caused by these tears of the discs.
These chronic lower back pain patients demonstrate central lower back pain that is aggravated by standing, lifting, impact sports and bending forward. Patients might gain relief by bending backwards while standing or relief by lying down. If there is no nerve compression, there typically will be no buttocks or leg pain present but occasionally disc pain can refer to the sacroiliac joint and even buttocks region without compression of a nerve root. Buttocks and thigh pain will not be the primary pain however but secondary (or lesser) pain that is not as intense as the central lower back pain. True lower back pain originating from the discs should typically be bilaterally equal or centrally located in the spine (with some exceptions).
Another source of lower back pain (which is the evolution or progression of degenerative disc disease) can occur from injury to the vertebral bone itself. If the disc fully degenerates, there is no shock absorption left and the endplate bone of the vertebra below starts to abut the opposing endplate of the vertebra above. With heavy activity, small fractures can occur in these endplates and the surrounding trabecular bone develops swelling (edema). These fractures are painful and can be aggravated by impact activities. In fact, many individuals will complain that after an impact activity (gardening, tennis, skiing, running and even cycling) they will “pay for it later”. What these patients mean is that they might have pain with the index activity but develop an intense delayed onset of lower back pain hours later after the event is over. Vibration is not well tolerated and even car or airplane rides can intensify this pain.
Lower Back Pain Generated from the Facets
The facets in the back of the spine can generate pain in the lower back. These structures generally are not typically the cause of as much lower back pain as the facets in the cervical spine are capable of generating neck pain. When the facets do cause pain, this pain mimics discogenic pain. It is estimated that about 10% of lower back pain is generated at least in portion by the facets. This type of pain may be one sided (unilateral) as the right facet may be painful while the left facet may not cause pain. This unilateral pain can be a clue to the origin of the pain but the differential of one sided central lower back pain includes a mildly inflamed nerve root on that side or a collapse of only one side of the disc.
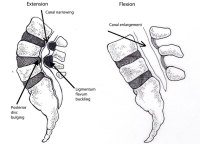
Facet pain is typically increased by extension as this increases the load on the joint surface. Flexion will unload the facet and commonly reduces the pain. Unfortunately, flexion can aggravate a facet capsule that is inflamed so the differential is not as easy to make using a physical examination.
Pars Interarticularis Generated Pain
The pars interarticularis is the region of bone that joins the superior facet to the inferior facet in the back of the spine (interarticularis means” in between the articulations” in English). The par interarticularis will fracture in some children and adolescents. In fact, about one in twenty adolescents will have developed this fracture by the age of 15. Most kids will not have significant initial symptoms or will ignore the initial symptoms and the back pain typically lessens, as these individuals get somewhat older. These pars fractures, left untreated generally do not heal but are also not symptomatic in the younger age groups.
These pars fractures can be quiet (asymptomatic) for years or even for the life of the patient. However, a simple action like a lift, a twist or a fall can tear the scar tissue at the old fracture site and thus activate pain receptors in the fractured area. The pain generated from this tear is generally difficult to distinguish from typical degenerative facet pain or disc disease. Extension (bending backwards) will increase the pain in many individuals and some people may develop additional leg pain. Rarely, leg pain without back pain can occur.
Sacroiliac Joint Mediated Pain
The sacroiliac joint can cause pain by itself but the sacroiliac joint is the most common region for referral of nerve pain and disc pain. It bears repeating that sacroiliac pain caused by the sacroiliac joint is uncommon. When these joints do cause pain, the pain is typically unilateral (on one side). Pain is aggravated by activities that produce stress in the joint such as lifting, lateral shifting (getting out of a car or off a bicycle for example) and bending.
Hip Pain
Hip pain classically locates to the groin. However some of the impingement syndromes (femoral-acetabular impingement) can cause lateral thigh pain and even buttocks pain. Activities that increase the pain are lateral movements ((getting out of a car or off a bicycle), climbing or descending stairs or walking on uneven ground.
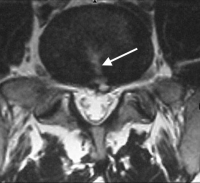
Stenosis Pain
Pain in the pelvis or lower back can be caused by neurogenic claudication. The symptoms of this condition are caused by the global compression of the entire sac of nerves in the lumbar spine (called the cauda equina as this group of nerves looks like a horse’s tail). Stenosis is the name used for narrowing of the central spinal canal and typically is caused by degenerative changes, bone spurs, shifting vertebra (degenerative spondylolisthesis) and hypertrophy (thickening) of the ligamentum flavum in the back of the canal. Central spinal canal stenosis therefore occurs with degenerative changes and aging. This type of lower back pain is generated by the global compression of all the nerves in the spinal canal and not just one individual nerve (which would cause leg pain).
The spinal canal changes in volume with spine positioning. With standing or walking, the canal actually narrows by as much as 30%. If there is a preexisting stenosis or narrowing of the canal, this 30% additional compromise will compress the nerve roots (cauda equina) in the canal. After a period from 2 minutes to thirty minutes (depending upon the seriousness of the compression), a dull ache, “numbness” and “drawing type pain” will occur in the base of the spine (in the sacroiliac joint or pelvis). The longer the individual stands or walks, the worse this pain becomes. With prolonged standing, the symptoms will start to travel down the legs, first in the buttocks and progressing down the thighs, occasionally radiating into the calves and feet.
Interestingly, some patients cannot stand for any length of time but can walk for extended distances. This is due to the fact that some patients bend forward substantially when they walk in a “controlled fall”. This position is enough to prevent the symptoms from occurring.
Relief for many patients will be obtained from bending forward, crouching down or leaning over a counter. The causes the spine to flex (bend forward) and relieves the pressure on the central sac of nerves. The famous “shopping cart sign” is considered a classic harbinger of this condition. Patients who cannot walk long distances due to these symptoms will love to go shopping at a super market as they can lean on a shopping cart and walk comfortably.
An easy differential to determine if this condition is present is to compare 30 minutes of walking to 30 minutes of riding a bicycle (stationary or road). Walking (or standing) should bring on these symptoms but the same amount of time spent on a bicycle should not cause symptoms. This of course is due to the fact that biking causes the spine to flex forward, which opens the canal and prevents the compression of the cauda equina. If lower back pain is present with cycling along with walking 30 minutes, the lower back pain is less likely to be caused by stenosis and more likely to be caused by degenerative disc disease.
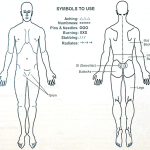
(Click to Enlarge Image) Body pain diagram. The patient fills this diagram out and reference to it gives information regarding the disorder.
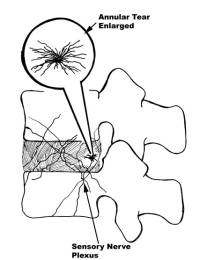
(Click to Enlarge) Tear of annulus causes ingrowth of vessels and pain nerves. These pain nerves will sensitize the disc which can increase back pain.
(Click to Enlarge Image) Axial MRI of annular tear. The white arrow points to the tear in the annulus and there is a small disc herniation at the end of the tear.
(Click to Enlarge Image) Isolated Disc resorption L5-S1- white arrow points to degenerated disc. Note the white signal in the vertebral bodies next to the degenerative disc. This is stress fracturing of the trabecula within the bone.

(Click to Enlarge Image) MRI of a degenerative facet- note white arrow points to slip of the joint. The lamina of this side points to the middle of the facet (crescent sign). Compare to the opposite side.

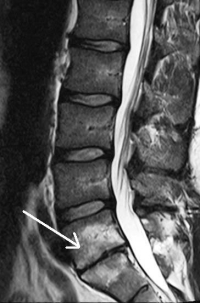
(Click to Enlarge Image) Isthmic Spondylolysthesis- arrow points to pars fracture. Note the slip of the L5 vertebra on the sacrum.

(Click to Enlarge Image) Stenosis as a result of aging- arrows point to disc bulge and ligamentum flavum hypertrophy.
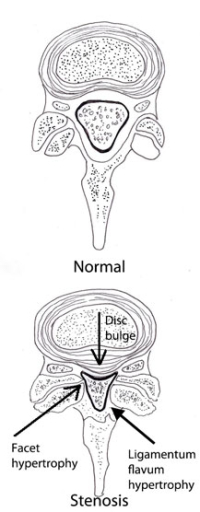
(Click to Enlarge Image) Normal and stenotic segments- black arrows point to hypertrophic facets, hypertrophic ligamentum flavum and to disc bulge.
Are you suffering from a common cause of lower back pain?
Would you like to consult with Dr. Corenman about your condition?
You can set up a long distance consultation to discuss your
current X-rays and/or MRIs for a clinical case review.
(Please keep reading below for more information on this condition.)
Degenerative Spondylolisthesis Mediated Pain
This condition could go under the degenerative disc disease column for creation of lower back pain but it really is an entity in and of itself. This condition occurs where the disc becomes degenerative and the facets also become degenerative at the same time. The global degeneration allows the vertebra to slide forward on the one below. This slide can allow lower back pain to occur but commonly can also cause central canal stenosis (see above).
This means that degenerative spondylolisthesis can cause both mechanical lower back pain just like degenerative disc disease and can cause stenosis-like lower back pain as noted in the stenosis pain section.
There is one more added possible symptom. Since all the vertebral stabilizers have worn out (discs and facets) and the vertebral segment can “slosh about”, there can be an “instability” type feeling regarding the lower back. This is a fear of loading the spine in certain positions as those positions will bring on a “shifting” sensation associated with pain.
Nerve Compression
Nerve compression pain is typically thought of by the general population as “sciatica”- sharp tingling pain that radiates down a leg into the foot. This is true but only tells part of the story. Patients with nerve pain that radiates down the leg can improve over time, even if they don’t require surgery. The pain abates by the centralization phenomenon.
This means that as the nerve becomes less inflamed, the pain is first eliminated at the end of the nerve distribution and then “centralizes” meaning the length of the track of pain region shortens or “moves up the leg”. For a patient with compression of the L5 nerve root, as the nerve heals- the pain is first eliminated from the foot. Over time, the calf pain disappears, then the thigh and buttocks pain fades away and finally the pain locates only in the sacroiliac joint on that side before the pain finally disappears.
If the nerve never becomes severely compressed but is only partially compressed, the pain generated may only radiate to the sacroiliac joint and never radiate down into the buttocks, thigh and so forth. This sacroiliac pain is commonly misdiagnosed by some individuals as originating from pathology in the sacroiliac joint but this is typically an incorrect assumption.
Unilateral sacroiliac pain can commonly originate from the discs of L4-5 or L5-S1. A mildly aggravated nerve root also commonly refers to this region. Interestingly, this inflamed nerve could be any of the nerves of the lumbar spine from L1 to S1 on that same side. Unilateral sacroiliac pain therefore has many different origins and has to be carefully worked-up if a surgical solution is to be considered.
Children can develop a herniated disc and will not typically develop leg pain. These kids will develop unilateral (one-sided) lower back pain or sacroiliac pain only. Children generally do not develop nerve related (sciatic) pain.
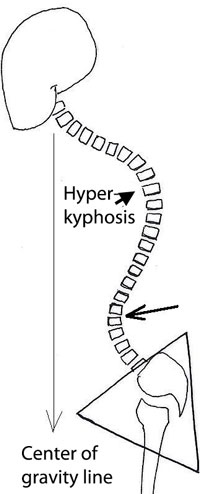
Hyperkyphosis Mediated Lower Back Pain (Scheuermann’s Disorder)
The thoracic spine is in the mid-back region of the spine where the ribs attach. The thoracic spine exhibits a normal curve called a kyphosis, which is a curving forward of the mid back. There is a condition called Scheuermann’s disease in which the vertebra of the growing spine in children can deform and change from little cylinders with parallel surfaces to wedges shaped structures. This deformity or wedging of the vertebra causes the normal curve of the thoracic spine to substantially increase (called a hyperkyphosis).
This increased curve in the thoracic spine has to be compensated by an increase in the lumbar spine curve or the individual will not be able to look forward while walking. Pain in the lower back can be generated by an increased compensatory curve (hyperlordosis) in the lumbar spine. This increased curve causes facet impingement syndrome where the pressure on the facets is greater than they can withstand and pain is generated with standing
Occasionally, the actual fracturing of the endplates of the vertebra in young individuals (which causes the wedging in Scheuermann’s disease) can be the source of lower back pain.
To learn more about common causes of lower back pain, please contact the office of Dr. Donald Corenman, spine specialist and back doctor offering diagnostic and surgical second opinions to patients in the USA and around the world.