Lumbar Fusion Types for Lower Back Pain Overview
Lower back pain is typically caused by a degenerative disc. As noted in the discussion of the anatomy and physiology of the disc (how the disc is designed on the microscopic level) in another section here on the web site, the disc develops degenerative changes as the nucleus (the jelly in the center of the disc) loses pressure and the wall of the disc (the annulus) tears. The back of the disc wall is filled with pain receptors and they send pain signals to the brain when this wall is torn. Most of the time, these signals are mild to moderate in intensity and they can be muted by physical therapy, core strengthening, certain activity restriction and non-steroidal medication to reduce the intensity of the pain.
The disc can continue to degenerate and develop “micro instability.” This causes abnormal forces to occur and chronically overloads the rings of the annulus. Multiple tears in these rings allow the disc to lose height and integrity. The inner jelly (nucleus) dries up further causing a drop in height. At this stage, the back can “go out” with certain activities but if these activities are avoided, the individual can live a guarded but acceptable life using the therapy noted above.
The disc can further degenerate and lose its ability to act as a shock absorber. In this case, damage to the bony endplate of the vertebra occurs as the endplate is overloaded with impact activity. This is an actual fracture of the endplate bone. Healing occurs but the cause of the fracture (the loss of shock absorption) is still present. Any activity in the next sixty days while the fracture is healing will disrupt the repair. Of course, no one is going to be placed in a body cast and lie perfectly still while the fractures are repairing themselves and the initial cause of the fracture (lack of shock absorption) is continuously present. Any activity will cause further injury to the endplate.
You can see how the endplates of the vertebra would be in a continuous state of repair and disruption with any activity- even the act of standing up! This causes chronic inflammation which is a setup for chronic pain. This condition is called isolated disc resorption (IDR). Not everyone with this exact condition has severe chronic lower back pain and some may even be pain free. The answer why will be Nobel Prize winning.
It should be noted that not every disc will follow this degenerative pattern and it is not inevitable that all discs will continue down this pathway. Even though the damage to the disc is permanent (there is no blood supply to heal the disc), most discs do not suffer the endpoint fate of IDR.
An important aspect of this condition is that even though the condition is significantly painful, it is not dangerous (as long as there is no concordant significant compression of the nerves in the spinal canal- a different story). This condition will not put the individual in a wheelchair or cause paralysis. The pain is similar to an arthritic hip or knee in that use of the degenerative area is painful and rest normally relieves the pain.
If the pain is stressing or disabling, the removal of the overloading forces and the repair of the vertebral integrity is essential to reducing pain. Bone is designed to transmit force without injury to itself. The purpose of fusion in the lumbar spine is to make a living bridge of bone from one vertebra to the next. This is a wonderful way to transmit force to the next vertebra by causing a fusion of living bone and eliminating the motion as the cause of the pain.
Now an argument is made that taking away motion of a segment will put stress on the next level up or down and there may be some truth to that. This is why the concept of the artificial disc replacement (ADR) was born. The idea itself is not bad but the current solution is still not ready for prime time. The reason is that the design of the artificial disc is not at this point a good reproduction of the normal disc that it is designed to replace.
The current ADRs do not have any shock absorption capabilities and do not dampen motion of the disc space as a normal disc would. The ADR’s lack of these normal discal characteristics puts more stress on the replaced segment than it was designed to tolerate. In addition, if there was substantial wear of the original disc space before surgical replacement, the artificial disc will still not relieve the lower back pain (damage to the other structures such as the facets). If there is an ADR surgically placed, over time, the vertebral bone can becomes osteoporotic (as in the elderly) and the artificial disc will fracture the endplate of the vertebra. This will cause the disc to subside into the bone. In addition, these discs have to be placed from the front through a belly incision which has its own potential complications. (See ALIF below).
Another important fact to consider in a much worn out disc level such as IDR is that there is very little motion in a worn out disc compared to a normal one. A fusion of this worn level will not worsen the stress on the levels above and below. There are a variety of lumbar fusion types to consider.
Lumbar Fusion Types
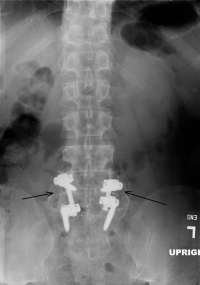
Lumbar fusion types are performed in various ways. Fusion can be performed as noted before from the front (an ALIF or anterior lumbar interbody fusion) from the side (an XLIF or extreme lateral interbody fusion), from the back (TLIF or transforamenal lumbar interbody fusion, PLIF) or posterior lumbar interbody fusion, or PLF or posterolateral lumbar fusion or from the front and back (a 360). Each fusion has its own indications and its own potential complications.
Anterior Lumbar Interbody Fusion (ALIF)
A fusion from the front of the lumbar spine (an ALIF) allows access to the disc to totally remove it and spread out or distract the disc space and restore normal anatomic height. Complete removal of the disc can be accomplished and a spacer can be placed to hold the alignment. The success rate of fusion is very good. The problem with anterior exposure is that the surgical approach is through the belly. Some of the abdominal muscles must be incised and the sack of intestines must be moved to the side. The aorta and vena cava and their branches must be moved to gain access to the disc spaces.
In males, there is a fine network of nerves called the sympathetic plexus that needs to be moved, especially at the lowest lumbar level. If these nerves become non-functional (1-5% of the time), the male can experience retrograde ejaculation. That is, the ejaculate will occur but will go into the bladder instead of exiting out the end of the penis. Both male and female may experience one warm leg compared to the other. This occurs when the same sympathetic nerve complex becomes damaged. These nerves regulate blood flow to the legs and damage to one side will allow blood to flow unregulated to the leg. Hence- that leg will feel warmer. Also, the procedure causes scar to occur. Any return visit to this surgical site is fraught with difficulty.
eXtreme Lateral Interbody Fusion (XLIF)
The XLIF is a procedure designed to have access to the front of the upper and mid levels of the spine (L1-5) similar to an ALIF without the dangers of an approach through the belly. The approach is through the side of the belly wall behind the intestinal sack and through the psoas muscle. The psoas is the muscle that flexes the hip joint- that is- the muscle that lifts the leg when ascending stairs. This muscle resides right next to the vertebral body in the front of the spine. Between the psoas muscle and the vertebral body lies the femoral and sciatic plexuses, the nerves that travel down to make the legs work. An approach through this area does put these nerves at risk for injury.
Posterolateral Fusion (PLF)
(Do not confuse with a PLIF) A posterolateral fusion (PLF) is one of the simplest and easiest fusions to perform. All that is required is a graft between the transverse processes and the facets. Normally, a set of screws and rods are used to stop motion which improves the fusion rate substantially. This fusion is indicated in patients that have lower demands on the fusion (a 75 year old with a sedentary lifestyle). If rods are not used, the procedure is called a “soft fusion” and there are times that this procedure may be indicated (a very sick patient that needs a fusion but could not tolerate a longer surgery). With instrumentation, the fusion rate is good and without, the fusion rate does drop. However, even a level without rods and screws that does not develop a full fusion (a pseudoarthrosis) may still be stable enough for this sicker individual.
“360” or Front and Back Fusion
A “360” is a front and then a back approach to get a 360 degree fusion. It combines an ALIF with a PLF. This procedure is probably the most complete fusion that can be performed but it requires extensive surgery that normally is not required. This procedure would be used in many cases for a failure of a prior fusion where the patient with an repeated surgery should have the “best chance” for success.
Posterior Lumbar Interbody Fusion (PLIF)
The PLIF, posterior lumbar interbody fusion (not a PLF- they are different procedures) is a procedure designed to create a fusion in the front and the back of the spine all through a small incision directly through the back of the spine only. The benefits are that the spine gets a “360” but the patient avoids an incision and approach in the belly. This technique is done by removing some of the medial facet on both sides to gain access to the disc space. There is a small area between the two nerve roots that allows access to the disc. This is a similar approach as a microdiscectomy. The disc is surgically cleaned out and fused through this approach on both sides. Fusion rate is very reliable and this technique allows solid fixation.
Transforaminal Lumbar Interbody Fusion (TLIF)
The last technique is called a TLIF, Transforaminal Lumbar Interbody Fusion. This is similar to a PLIF, but the access to the disc is performed only on one side. This involves a total removal of the facet on one side. The benefit of this is twofold. First, it allows a greater working space between the nerve roots (double that from a PLIF) and therefore much less pressure on the nerve roots to gain access into the disc space. Second, the removed facet acts as the bone graft which means that no “hip graft” needs to be taken. The success rate for fusion is very good.
The TLIF and PLIF are very similar fusions. In either case, both an anterior fusion and posterior fusion can be done from a small incision from the back of the spine. The risks are of heterotopic bone formation (bone forming in the wrong place) and nerve root irritation, more so in the PLIF than TLIF.
Minimally Invasive Lumbar Fusion (MIS)
There is a lumbar fusion type of approach called “minimally invasive lumbar fusion” or “MIS”. This is not a type of fusion but an approach that can be used with the PLIF or TLIF. The purpose of this type of approach is to “preserve” the muscles around the segments being fused. There is noting wrong with the procedure but the problem with this concept is that these muscles (the multifidi and transversalis) are segmental muscles that insert from vertebra to vertebra. Since the two vertebrae are going to be fused together, there is no reason to preserve these muscles and actually significant reasons to move them.
In general, the greater and thicker the bony surface area for fusion, the greater the success and solidity of the fusion. Preserving these two muscles does nothing for any type of stability as these muscles cross the two vertebrae involved in the fusion and will not have any function after the fusion. Remember that the fusion is designed to stop the two vertebra’s motion. In addition, these muscles take up spots on the vertebra that need to be exposed to allow bone to grow. Moving them allows greater surface area for bone growth.
One of the claims of MIS is that the incisions are smaller than MIMS (minimum incision microsurgery). However, if you add up the length of the necessary incisions for the “minimally invasive fusion”, they are in total longer than a MIMS procedure. Because of the location of the MIS incisions, the incisions tend to spread apart more and have less cosmetic appeal.
Minimal Incision Microsurgery (MIMS)
Minimal Incision Microsurgery (MIMS), just like the MIS, is an approach and can be used with the TLIF or PLIF. The incision is made in the center of the spine and gives access to the fusion area and the central canal. This access allows a full decompression of any herniation or bone spur along with excellent exposure for fusion.
For more information on lumbar fusion types for lower back pain, please contact Dr. Donald Corenman, spine surgeon and back pain specialist in the Vail, Aspen, Denver and Grand Junction, Colorado communities.