EMGs and NCVs are electrical tests to help diagnose problems that can occur in the peripheral nervous system. There are some basic problems that can be easily diagnosed and some disorders that these tests cannot easily distinguish apart. Radiculopathy (compression of the nerve root in the spine), neuropathy (dysfunction of the nerve in the arm or leg), some forms of multiple sclerosis and some other nerve diseases can be demonstrated by the EMG/NCV. However, if only pain and/or sensory changes develop from nerve compression without motor involvement, the EMG/NCV is less useful as it will probably not identify this disorder.
EMG and NCV testing will not be helpful to diagnose problems that originate from the central nervous system (CNS). For example, if compression of the spinal cord causing myelopathy is present (see website), the EMG/NCV test will not be sensitive to this condition and will not be diagnostic.
Two types of specialists, neurologists and physiatrists normally perform these tests. Unlike an MRI, the results of these tests are not necessarily specific. That is, the results are interpretable. The experience and skills of the tester can significantly impact the quality of the examination. The information gained may be quite valuable or occasionally add confusion to the diagnosis.
The structures that can be tested are large motor and sensory nerves, neuromuscular junctions and the muscle cells themselves. One cannot easily test sensory roots at the dorsal root ganglion (DRG) in the spinal canal and small sensory and autonomic fibers. Pain fiber nerves are very small diameter nerves and cannot be tested. This means that a patient can have pain and paresthesias (pins and needles) but the nerve testing will be normal. Another way to put this is that a normal test does not mean the patient does not have nerve pathology or pain.
These tests are most useful if you suspect a peripheral neuropathy (disease of the nerves of the legs) or disease processes like Charcot Marie Tooth, a rare genetic nerve problem.
NCV- Nerve Conduction Velocity
To understand what the nerve conduction velocity (NCV) tests, you need to understand the physiology of the nerve as it relates to nerve testing.
After a stimulus to a nerve ending occurs such as a touch receptor in the finger, a normal nerve conducts the signal up its length at a certain set speed. A nerve that is compressed will have its signal speed slowed at the site of compression. The compression can be significant enough that the signal may be completely stopped. Severe compression may actually kill a portion of the nerve or the nerve itself. Damage may injure the sheath that surrounds the nerve (the myelin sheath) creating a block to conduction but leaving the nerve itself intact.
This then leads to the fact that if you could generate a test signal up or down the nerve, you could measure the speed of the nerve’s conduction. It turns out that this test signal can be generated by a simple electrical stimulus and the conduction wave measured by electrodes on the skin further down the nerve pathway. This is called the NCV or nerve conduction velocity. Nerves will conduct in both directions when stimulated by an electrical stimulus regardless of the “normal” direction. You can stimulate the upper end of the nerve with an electrical charge and measure the speed that the signal travels down the nerve.
This investigation is therefore useful for entrapment of peripheral nerves in the arms and legs. Many are familiar with the terms carpel tunnel syndrome and cubital tunnel syndrome (entrapment of the nerve in the wrist or elbow) but there are many other areas in the upper or lower extremities that can compress these nerves as well.
To check conduction of the nerves of the arm, placement of a stimulatory electrode band on the upper arm is performed. “Receiver bands” that read the descending signals are placed before the wrist, on the palm and on the fingers. The distance between the stimulating electrode and each receiving electrode is physically measured and entered into a computer. When the stimulatory electrode triggers a stimulus on the upper arm, the signal propagates down the nerve. The computer measures the time it takes for the signal to get to each subsequent electrode. The computer then calculates the speed of conduction. If the nerve is compromised, the speed will slow at the point of compression and the computer will note it.
This scheme works for any nerve that has its proximal and distal ends accessible to electrodes. A disease process called peripheral neuropathy occurs where the membrane of the nerve malfunctions due to vascular or internal insult. The signals that propagate up the nerve become disturbed and symptoms of foot burning and numbness ensue. The NCV is very useful to determine if this problem exists. Slowing of the signal at various points would clue in the electromyographer to this condition.
The downside is that if the peripheral neuropathy involves only the small diameter nerves (which commonly can occur), these small nerves are not tested by the NCV and the test will be negative (showing no abnormality when one really exists).
Would the NCV work for identification of compression of the nerves that exit the spinal canal such as in the case of a herniated disc? The answer is no, as obviously you cannot introduce a stimulatory electrode above the compression into the spinal canal to stimulate the nerve without harming all the structures around it.
The H Wave
There is a way however to check these spinal nerves utilizing an NCV-like stimulus without the need to stimulate in the unreachable canal. This technique uses the unusual fact that an electrical stimulation in the middle of a nerve can deliver the signal in both directions, even though it was “designed” to carry a signal only one way.
Stimulation of the nerve in the leg can cause this signal to travel up the sensory nerve to the end at the dorsal root ganglion in the spinal canal and then “bounce” back down the same nerve to the measuring electrode. This is similar to measuring an echo. You can measure the time this nerve echo returns just like measuring a normal conduction wave. Again, there is a normal conduction velocity and therefore measuring this echo should have a normal travel time based upon length of the nerve. Anything over this normal echo time could indicate a slowing. This slowing could be from nerve compression in the spinal canal (herniated disc).
The problem with this echo is that it is a very weak signal and hard to pick up on testing due to the present ambient “noise” recorded on the NCV. In addition, measuring the distance this impulse has to travel is an estimation and not an actual measurement. To add confusion to this test, any patient who is heavy or edematous will preclude success with the H wave. Patients who are “fidgety” have problems with this test and even the room temperature can change the results of the test.
The F Reflex
The similar principle works for the F reflex as it does for the H wave. The difference is that the F reflex goes up through the spinal cord and doesn’t reflect back. The signal instead travels through the reflex arc just as the ankle jerk reflex and comes back down through the motor nerve. This is essentially an electrical test for the Achilles reflex (S1 nerve). The same problems that can occur with the H wave occur here. Again, the F reflex is difficult to test because the waveform is so small.
Other than the H and F reflexes, there are no other NCV values that can check the integrity of the spinal nerves. This leads to the other part of the test, the EMG.
EMG (Electromyogram)
The EMG or electromyogram is a complementary but different test to the NCV. Here, the actual muscle is tested instead of the speed of conductivity of the nerve. An understanding of how and why the muscle reacts with normal, incomplete and complete nerve injuries is necessary to understand the products of this test.
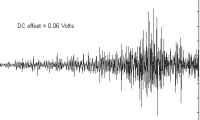
This EMG test involves a probe as small as an acupuncture needle inserted into the tested muscle. When the needle touches the muscle membrane, it registers crude muscle activity. This electrical recording is initially measured with rest activity and then with active voluntary contraction (recruitment).
There is a specific pattern that is recorded for normal muscle. Normal muscle is quiet at rest. When voluntarily contracted, there will be a smooth escalation of increased signal spikes until maximum contraction is achieved. This is due to the “all or nothing” law of muscle contraction. Each muscle cell either contracts fully or not at all. When greater strength is necessary, the brain recruits more muscle cells in the same muscle belly for more strength (force of contracture).
The “fine motor skills” we all exhibit have to do with the brain selecting each small group of muscle cells to fire individually. Only a small amount of muscle cells contracting will yield a fine motion up to a full contingent of cells contracting which is ultimate strength. The fine “ticks” noted on the EMG record every small “all or nothing” contraction of each muscle cell in the recording electrode’s vicinity. As more muscle cells are recruited, there are more and more spikes in a smooth unbroken ascending pattern recorded.
To understand how motor nerve injury would be “seen” by an EMG, you need to know that the motor nerve does not insert directly into the muscle. There is a space or synapse between the nerve and muscle called the motor endplate. The end of the nerve at this motor endplate contains the chemical (acetylcholine) that when released, will stimulate the muscle to contract. There are receptors for acetylcholine on the muscle side of the endplate. A muscle that has lost its nerve supply will not be exposed to any local acetylcholine and in response, will become irritable.
Eventually this muscle cell that has lost its nerve supply becomes very irritable and starts to “twitch”. These small “wormy” contractions look very different than the normal “all or nothing” contractions. These can be picked up by the EMG and are called positive sharp waves and fibrillation potentials. These findings indicate loss of the nerve contact with the muscle.
It takes two to three weeks after the nerve is injured to develop these fibrillations and sharp waves. Therefore an EMG prior to this golden two to three week period will not reveal changes and be much less effective for diagnosis in a deinnervated muscle.
Muscles that have lost their nerve supply not only become more irritable, but also send out a chemical called a neurochemotactic factor. This is really a chemical cry for help. Any intact motor nerve near this non-innervated muscle can send out a new branch that will eventually connect with this muscle. This action is called budding or sprouting.
The muscle will now contract again under the influence of this new nerve supply. Budding takes between ten to sixteen weeks after nerve damage to occur and one nerve can bud up to ten times. If there are enough new sprouts, the contraction amplitude will be bigger but much more un-uniform on the EMG. This is picked up by the EMG as coarse contractions and increases the evidence that there has been nerve injury and re-connection.
Testing Limitations
If you understand what has been previously discussed, you have realized that we can only measure the conductibility of the large nerves after they originate from the spinal canal. The ability to measure the pain nervous system is not possible. We cannot measure compression of the nerve root in the spinal canal. Here is where the EMG/NCV breaks down. A patient with severe leg pain but no motor nerve injury (a common scenario) will have a relatively normal test.
Also, a patient with central stenosis (neurogenic claudication-compression of all the nerves in the spinal canal) or even leg pain from lateral recess stenosis will not have a permanent nerve injury but a dynamic injury. This is temporary nerve compression that does not lead to permanent changes in the nerve itself. No findings on EMG/NCV will be found.