Earlier this month, Donald S. Corenman, MD, DC et al.1 received notification that one of his recently-completed research studies was accepted for publication by Spinal Research peer-reviewed Journal, SPINE. The independently-analyzed study, entitled, BMP-2-Augmented Transforaminal Lumbar Interbody Fusion (TLIF) for the Treatment of Chronic Low Back Pain Secondary to the Homogeneous Diagnosis of Discogenic Pain Syndrome: Two-Year Outcomes, describes the results of Dr. Corenman’s standard fusion surgical technique, TLIF, for the treatment of one of the most mysterious and disabling low back disorders out there: lumbar discogenic pain syndrome (DPS). (Figure 1)
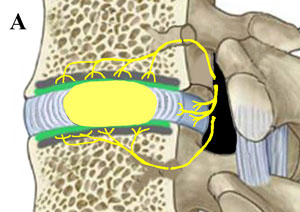
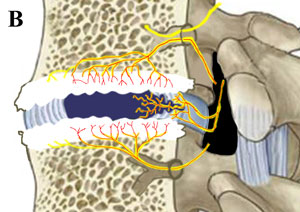
Figure 1. Side-Cut-a-Way View of a Normal Disc versus a Disc Affected with Discogenic Pain Syndrome (DPS)
 |
 |
|---|---|
| Figure 1a: Here is an example of what a normal disc and its surrounding vertebra should look like. Note the amount of nerve fibers that surround the disc but do not greatly penetrate it. These nerve fibers (sinuvertebral and basivertebral nerves), are known to have the potential to carry pain signals to the brain when inflamed and irritated, which can occur following a special type of disc degeneration and disc tearing. | Figure 2b. Here is an example of discogenic pain syndrome. Note that the disc has collapsed and ripped open toward the back. This tearing (called an annular tear) has allowed pain-carrying nerve fibers to grow into the center of the disc, effectively wiring the disc for pain. Also note the increased nerve fibers in the vertebral endplates surrounding the disc, which wires the endplates for pain. Because of biomechanical and biochemical mechanisms, these nerves are now constantly inflamed/irritated and sending pain signals to the brain in patients who suffer DPS. |
Study Design
After searching through the registry of 257 consecutive TLIF patients, all in whom were operated upon by Dr. Corenman for the chronic unrelenting low back pain of DPS, the target study group of 45 patients was reached. All of these patients had a solitary diagnosis of DPS, and patients with other common diagnoses (i.e., spondylolisthesis; spinal stenosis; scoliosis; radiculopathic or recurrent disc herniation; or instability) were removed from the study. All patients completed standard quality-of-life questionnaires (QOLQs) before the operation to establish a baseline of their condition. The QOLQs, which included the Oswestry disability index (ODI), Physical Component Summary Score of the Short Form-12 Health Survey (SF12-PCS) and a 0- to 10-point numeric rating scale for low back pain (bNRS), were again collected at least two years after the operation and then statistically analyzed in order to determine how much improvement the patients had made following the surgery. A 0- to 10-point patient satisfaction scale and return to work questionnaire were also completed at a two-year minimum. Data concerning perioperative surgical complications and revision surgeries were also gathered.
Results
At an average postoperative follow-up of 41.9 months, 36 patients had completed the postoperative QOLQs (36/45, 80%), which were statistically analyzed by SPRI. There was statistically significant improvement following surgery as measured on all QOLQs. (Table I) Noteworthy was a greater than 40% improvement with regard to the ODI and bNRS where the average postoperative scores were 21.4 (0-100 scale, where 100 is severe/complete loss of function with regard to the activities of daily living) and 2.6 (0-10 scale, where 10 is severe in-the-hospital pain intensity), respectively. Patient satisfaction scores rated very high, as a median score of 9 out of 10 (10 = complete satisfaction) was calculated and 84.4% of the patients were able to return to their preoperative job, with or without limitations. (Table II) 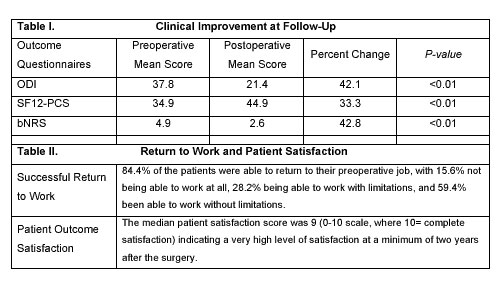 There were four revision surgeries needed over the 3.5 year follow-up interval, which included two for removal of instrumentation, one for decompression of a cage that had slid somewhat out of place, and the last one for the development of adjacent level DPS, in which the fusion was extended up one level. There were no serious perioperative complications and all patients achieve successful solid fusion. There were no serious complications from the use of BMP-2.
There were four revision surgeries needed over the 3.5 year follow-up interval, which included two for removal of instrumentation, one for decompression of a cage that had slid somewhat out of place, and the last one for the development of adjacent level DPS, in which the fusion was extended up one level. There were no serious perioperative complications and all patients achieve successful solid fusion. There were no serious complications from the use of BMP-2.
Discussion
This published study is the most comprehensive clinical outcome study ever performed on patients with the stand-alone diagnosis of discogenic pain syndrome (DPS) and the patient-outcomes at a minimal two-year follow-up were quite pleasing to Dr. Corenman and his team. There is a recent push in the world of spine research to no longer ignore the patient’s own opinion of the surgical results, and an increasing number of high-impact peer-reviewed journals are making the patient’s opinions mandatory (typically, through the category of patient-satisfaction). In the design of his study, Dr. Corenman did not shy away from this topic and allowed his patients to speak out in the paper. And speak they did, as they reported a median patient satisfaction score of 9 on a 0- to 10-point scale, where 10 indicated complete, 100% satisfaction at a minimum of two-years after the surgery (most patients that reported outcomes were almost 3 ½ years status post-surgery). Dr. Corenman attributes this unusually high patient satisfaction, as well as the success of the TLIF procedure for the treatment of DPS to two things: #1) the very specific diagnostic work-up that he uses, which has been honed over his 26-year career as a board-certified, fellowship-trained orthopedic spine surgeon, to make sure each patient is an ideal candidate for the surgery, and #2) patient education: Patients should not have unreasonable expectations about the typical results of any fusion procedure. Typically patients will have permanent limitations following the surgery and are always warned about risks of re-injury secondary to doing things such as very heavy lifting or continue participation in very arduous activities. By utilizing this strategy, Dr. Corenman has developed a very successful surgical treatment for the fairly rare but often devastating diagnosis of discogenic pain syndrome.
Conclusions
Dr. Douglas Gillard, head spine researcher of the Steadman Philippon Research Institute, concluded his analysis of the results by saying, “Although limited by retrospective design and small cohort, the results of this investigation suggest that BMP-2-augmented TLIF is a reasonable treatment option for patients who experience discogenic pain syndrome and affords high patient satisfaction.” *Note: this publication’s abstract is now avaliable for free viewing on PubMed.com: TLIF Study Abstract. The entire publication is avaliable for purchase at Spinal Research’s number one peer review Journal, SPINE: TLIF Complete Study.
