Rheumatological Conditions that Affect the Spine
Spondyloarthopathies (spondylo=spine, arthros=joint, pathos= condition of)
Rheumatological conditions that affect the spine are due to autoimmune disorders that attack the musculoskeletal system. In a normal immune response, alien proteins such as those of bacterial or viral origin trigger the immune system to destroy the invading organism. In an autoimmune disorder, the immune system becomes confused and develops sensitivity to normal body proteins. When the immune response mistakenly identifies these normal host proteins as “foreign invaders”, inflammation, swelling, erosion of bone, joint and nerve destruction can occur. This is the basis of an autoimmune spinal disorder.
Symptoms of Autoimmune Spinal Disorders
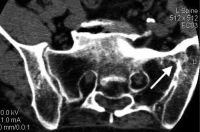
With the exception of rheumatoid arthritis, many autoimmune spinal diseases start with sacroiliac joint (SI) involvement, the joints in the back of the pelvis. One of these diseases (ankylosing spondylitis) attacks the SI joint bilaterally (on both sides) but most of these disorders only cause unilateral (one-sided) SI joint injury.
The classic first symptoms are pain and stiffness in the morning that disappears with activity. Fatigue is also a common symptom of these rheumatologic conditions that affect the spine. Stiffness that disappears with exercise is very typical for spinal autoimmune disorders. Be forewarned that lumbar degenerative disc disease can also display similar symptoms.
Rheumatoid arthritis, psoriasis, ulcerative colitis, Crohns disease, Reiter’s syndrome, ankylosing spondylitis, lupus (SLE), myositis, polymyalgia rheumatica, and DISH (diffuse idiopathic skeletal hyperostosis) are some of the spondyloarthropathy diseases associated with spine pain and stiffness.
X-Ray Findings of Spondyloarthopathies
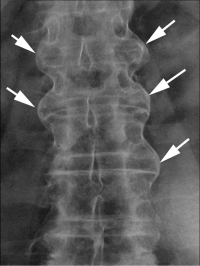
X-rays can demonstrate classic findings for these rheumatological conditions of the spine. Syndesmophytes are bone spur formations that develop off the upper and lower edges of the vertebral bodies. They can be categorized as marginal or nonmarginal.
Marginal syndesmophytes are bone spurs that originate immediately out of the edge of the body and connect one vertebra to another thru the “margin” of the vertebra. Marginal syndesmophytes stay within the confines of the anterior and posterior longitudinal ligaments and are specific for ankylosing spondylitis. The spine develops the appearance of segmented bamboo so is called a “bamboo spine.” In the early stages, the normally “scooped” or curved front of the vertebra “fills in” with bone to become “square”.
Nonmarginal syndesmophytes appear as large spurs or “parrot beak” spurs and grow out of the corners of the vertebra. These spurs normally occur with spine involvement in psoriasis, ulcerative colitis, Crohns disease, Reiter’s Syndrome, and DISH.
Sacroiliac joints are the first joints to be involved with many of these disorders (except DISH). By using X-ray only, involvement of these joints can be difficult to diagnose. The edges of the joints may become blurred and occasionally the joint fuses and “disappears” on X-ray. Again, if the sacroiliac joint is involved, bilateral involvement characterizes ankylosing spondylitis and unilateral involvement covers most of the other inflammatory disorders. The MRI is the most sensitive scan to determine if the sacroiliac joint is inflamed.
Are you suffering from a rheumatological condition that affects the spine?
Would you like to consult with Dr. Corenman about your condition?
You can set up a long distance consultation to discuss your
current X-rays and/or MRIs for a clinical case review.
(Please keep reading below for more information on this condition.)
Rheumatoid Arthritis (RA)
It is estimated that 1–2% of the world’s population has rheumatoid arthritis. This disease attacks the synovium lining of diarthrodial joints. Diarthrodial joints are the common joints we all think of such as the shoulder or knee. The facets in the spine are diarthrodial joints and there are more of these joints in the spine than all the other joints in the body. The junction of C1 and C2 at the base of the neck is also a diarthrodial joint.
The basis of this disease is the immune attack of the synovium lining of the joint. The synovium is the thin layer of cells in every joint that produces the oily fluid that lubricates the joint, As noted before, the spine contains multiple diarthrodial joints (the facets and the atlanto-dens articulation of C1-2). Rheumatoid arthritis can affect all these joints.
Onset typically occurs symmetrically (on both sides) and the disease typically involves the hands at the early stage. Swelling and pain of the finger joints signals the onset. Painful nodules can form subcutaneously (under the skin), and the fingers will appear “windswept” (dislocated or subluxed all in one direction) in later stages.
The disease also affects other body systems such as the blood vessels (vasculitis) and nerves. The lungs can be affected as well as the pericardium (lining of the heart).
Nerve involvement can occur. Mononeuritis multiplex symptoms can develop. These are multiple occurrences of single unrelated nerve injury/involvement (ex: tibial nerve on the left leg and the median nerve on the right arm). The vascular supply to the nerve is damaged, starving the nerve of oxygen.
With a well-known disease process such as rheumatoid arthritis, you would assume that there should be one lab test to determine if the patient has the disease. That however is not the case. Some of the diagnostic tests positive in RA, such as the rheumatoid factor test, show up in 3% of the healthy population.
When RA affects the spine, the cervical spine is most commonly affected. Only rarely does the thoracic or lumbar spine become involved. With spinal involvement, the symptoms almost always start with stiffness and decreased range of motion of the neck.
Rheumatoid arthritis is a destructive disease that may have obvious X-ray findings in later stages. RA destroys the synovial joints so X-ray will reveal that the bone of the facets has become eroded. The vertebral bodies and discs will have no involvement.
A synovial joint exists between the dens (the top of C2) and the arch of C1. The disease can therefore produce C1-2 instability by eroding the dens or the transverse ligament. This creates an increase of the space between the two bone surfaces on the lateral cervical X-ray.
Commonly, degenerative spondylolysthesis (slip of one vertebra on the other) of the cervical vertebrae occurs with this disease process.
Seronegative Spondyloarthopathies
Seronegative spondyloarthopathies are called this due to the lack of the ability of any specific blood tests that can reveal the presence of these disorders (seronegative means no positive blood testing). The presence of these disorders is revealed by symptoms, findings on MRI and X-rays and non-specific blood testing. Non-specific blood testing means that certain blood test findings are present in these disorders that can also be present in any number of disorders. It is the combination of all these findings that reveal the presence of seronegative spondyloarthopathies.
The seronegative spondyloarthopathies are enteropathic arthritis, psoriatic arthritis, and Reiter’s syndrome. These diseases have many features in common, such as unilateral involvement of the sacroiliac joint, nonmarginal syndesmophytes (“parrot beak” bone spurs that grow on the side of the vertebral bodies), and fatigue/lethargy. Many patients with these disorders will have an HLA-B27 allele on one chromosome (a gene found on DNA strands). Just like in rheumatoid arthritis however, HLA-B27 is found in the normal population; so it is not by itself diagnostic if present.
Differential from Degenerative Disc Disease
Morning stiffness is the hallmark of spondyloarthopathies. Morning stiffness can also be associated with lumbar degenerative disc disease (DDD) and stenosis. Patients with all three diseases have reduction of lower-back pain with a hot shower and some stretching, but the patient with spondyloarthropathy will feel significantly better.
The DDD patient will have increased symptoms with exercise and the spondyloarthropathy patient will tolerate the increased activity without significant problems. The spondyloarthropathy patient may have symptomatic improvement with exercise. Sacral or central lumbar pain will be present in both. Spondyloarthropathy disorders are not normally associated with leg pain where DDD can have leg pain associated. Reiter’s patients may complain of heel pain.
Ankylosing Spondylitis
The prototype for autoimmune spinal disorders is ankylosing spondylitis (AS). This is a disease process that causes the spine to fuse together over time. Found generally in younger males, AS has classic prodromal symptoms. The diagnosis may not be identified for months after the onset of initial symptoms. The incidence of this disease is one in every thousand Caucasians. Females can also succumb to AS. The blood marker HLA-B27 is common with this disease, but its presence does not absolutely predict disease, and absence does not assure the lack of disease.
Young adult males will develop prodromal symptoms (symptoms that occur before full manifestation of the disease) such as morning stiffness and pain in the lower back (sacroiliac involvement). Sleep can be difficult. Some patients will develop iritis, an inflammation of the anterior chamber of the eye. This disease is cyclical. That is, ankylosing spondylitis is noted for exacerbations and remissions. Again, think of this disorder in a young adult male, if symptoms include morning stiffness that improves with activity.
Reiter’s Syndrome
Reiter’s syndrome is associated with either a sexually transmitted disease—chlamydia—or onset of a bacterial intestinal infection. After the infection ceases, the syndrome begins. The triad of symptoms consists of urethritis (inflammation of the urethra), conjunctivitis (inflammation of the white of the eye), and arthritis (pain in the joints). This syndrome includes the hallmark of the disorder, heel pain and swelling, most likely resulting from an inflammation of the insertion of the Achilles tendon or the planter fascia. Back pain from sacroiliac joint involvement (sacroillitis noted above) occurs in 70% of patients, and inflammation of the eye, conjunctivitis occurs in 40% of patients, Myalgias can occur, and sausage digits (highly swollen fingers) are also is seen with Reiter’s syndrome.
Psoriatic Arthritis
Psoriasis is primarily known as a skin disease. The skin on the extensor surfaces become reddened and develop a silvery flaky scale. A small percentage of patients develop arthritis. Psoriatic arthritis and spondyloarthropathy are associated with changes in the nail beds of the fingers. Sausage digit can be noted in some patients.
If a patient with psoriasis develops arthritis, 95% have peripheral joint involvement (elbows, knees, and hips); and 5% have spinal involvement, including sacroiliac involvement and the typical nonmarginal syndesmophytes.
Enteropathic Arthritis
These disorders are intestinal borne. The two most common diseases associated are Crohn’s disease and ulcerative colitis. Both involve intestinal debilitation, and both are known to involve the spine. Ten to twenty percent of patients will develop sacroiliac involvement, and 10% will develop spondylitis or spinal inflammation.
Myalgias and Fibromyalgia
Myositis and Myalgias
There are some unusual diseases that cause muscle-generated pain, such as polymyalgia rheumatica and myositis. These are systemic autoimmune diseases related to temporal arteritis. In these cases, the immune system attacks muscle proteins. Patients with this disorder have debilitating muscle aching. The common flu also causes temporary generalized muscle pain (myalgias) by a similar but temporary mechanism.
Fibromyalgia
Fibromyalgia is a controversial diagnosis as there are no lab tests, X-rays, or other concrete ways to prove this disorder exists. This diagnosis is made by excluding any other potential diagnoses and then inventorying the patient’s complaints to see if these fit with fibromyalgia guidelines.
The most common patient is a female of childbearing years. This syndrome tends to get somewhat better with activity but most patients will have not engaged in exercise as this causes soreness and fatigue. These patients complain of stiffness and lethargy. Headaches, irritable bowel syndrome, and sleep disturbances are quite common; and this disorder is regularly associated with depression. For diagnosis, pain should be noted in all four quadrants of the body: legs, arms, pelvis, and central core, with eleven of eighteen “tender points” present in specific areas. Treatment is similar to that of chronic pain syndromes but exercise is essential to treat fibromyalgia.
For additional resources on rheumatological conditions that affect the spine, or to discuss treatment options for autoimmune spinal disorders, please contact Dr. Donald Corenman, spine surgeon and neck specialist offering diagnostic and surgical second opinions to patients in the USA and around the world.