Chronic Radiculopathy Overview
Nerves are persnickety creatures. They can generally tolerate some compression but don’t really like to be pushed around. Unfortunately, there are many conditions of the spine that cause nerve compression in the spine. A herniated disc of the spine, spinal central stenosis, lateral recess stenosis, and foraminal stenosis, as well as foraminal collapse, are but a few of the compressive conditions that can cause nerve pain leading to lower back pain and leg pain.
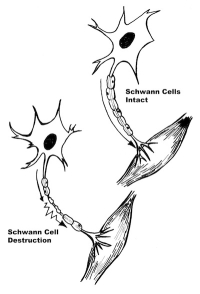
Even though there are many occasions where severe nerve compression in the spine causes no long term after effects, it can occasionally permanently damage the interior workings of the nerve. A decompression surgery of the nerve (microdiscectomy of the lumbar spine or lateral recess decompression) will generally take the pressure off the nerve and in 90-95% of the cases the nerve will recover.
What about the other 5% of cases where persistent lower back pain is common? If there is no further compression of the nerve (a new MRI after surgery in the face of continuing pain demonstrates no further nerve compression in the spine) and there is not a pinched nerve in the spine or no instability of the spine within the segment that can cause intermittent mechanical compression, then these symptoms represent chronic non-healing injury to the nerve root or “chronic radiculopathy”.
Stretch can also lead to a nerve injury of the spine leading to nerve pain, lower back pain, and leg pain. This is much more common in the arm where “stingers” are stretch injuries of the brachial plexus (the shoulder nerves) but the sciatic and femoral nerves in the legs can also be stretched and injured. A nerve injury in the spine can occur from sports, impacts and even rarely, slip and fall accidents.
Are you suffering from symptoms of Chronic Radiculopathy?
Would you like to consult with Dr. Corenman about your condition?
You can set up a long distance consultation to discuss your
current X-rays and/or MRIs for a clinical case review.
(Please keep reading below for more information on this condition.)
Post-Surgical Non-Pain Related Nerve Symptoms
If surgery is warranted to decompress the nerve, some patients may observe unusual symptoms in the leg after surgery. With the intense pain now gone, patients can experience some symptoms that were present prior to surgery but were not noticed because the preexisting intense pain from nerve compression overshadowed these symptoms. Some will complain of “bugs crawling” and others will be sure that someone spilled cold water on their leg but when they glance at their leg- it is dry. This alteration of symptoms (referred to as spinal cord dysfunction) will most likely eventually disappear but it may take as much as six months.
Mechanics of Nerve Injury and Spinal Cord Complications
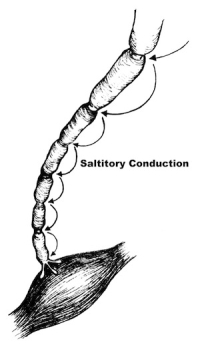
The nerve root is a compilation of sensory and motor nerve cells. Any nerve cell is simply a long tube that connects the brain to the end point structure (the foot, thigh, buttocks, hand, shoulder, etc.). In fact, the nerve cell is the longest cell in the body with some reaching up to three feet in length. These structural tubes are made of membranes with “pumps” that continuously push potassium and sodium into and out of the cell to maintain a charge of electricity across the membrane. This electrical charge is what allows the signal to travel up or down the nerve.
If the membrane of the cell is damaged and becomes “leaky” or the blood vessel that services the nerve membrane pump is injured, the cell membrane will become dysfunctional. That is, the nerve may deliver a signal to the brain even though the sensor on the end of the nerve doesn’t trigger it (an ectopic focus) or block a signal that should have been transmitted. If the nerve carries ectopic pain signals, the brain perceives pain. If the ectopic signal is from a proprioceptive nerve (position sense), pins and needles sensation will be perceived by the brain. If the motor nerve is injured, the muscle attached to that nerve will be weak and if the nerve is in the leg, a limp may be noticed.
This means that in the face of a pain nerve injury, nerve impulses will travel up to the brain on a fairly constant basis. Pain can be described as constant “burning”, “raw” and “gnawing”. Hypersensitivity of the skin (hyperalgesia or allodynia) can occur. A simple brushing of bed sheets on exposed skin can cause intense pain. This is referred to as peripheral neuropathy.
A good example of this phenomenon is “phantom pain syndrome”. Some unfortunate individuals with an amputation of the leg will still complain of “foot pain”. The nerve at the amputation site still conducts an impulse and the brain is wired to perceive “foot pain” even though there is no foot!
This type of chronic neuropathic pain can be managed and controlled with medications and nerve stimulation. Years ago, Melzak and Wall won a Nobel Prize when they introduced the “gate theory of pain”. We all have unknowingly used this discovery when we were kids. When our arm or leg was injured, we would vigorously rub the skin of the injured area and the pain would disappear. What would be occurring is that our stimulation of the skin would “flood” the sensory system and the “gate” to the pain pathway would be “closed”.
The TENS unit (transcutaneous electrical neural stimulation) works off this principle. Pads placed on the skin conduct an electrical signal from a small generator, which blocks the pain signal. This stimulator substitutes the electrical stimulation of the skin for the intense skin rubbing and actually substitutes “white noise” for pain perception.
An implanted spinal cord or implanted peripheral stimulator uses this same technique to reduce pain. Stimulation of the skin or spinal cord floods the sensory system and is designed to reduce pain. Implanted stimulators tend to have better signal production and can reduce pain much more than TENS units but of course, require an operation for implantation.
If you are experiencing ongoing, persistent symptoms associated with a pinched nerve in the leg, nerve compression in the spine, or if you are chronically suffering from leg pain, lower back pain and nerve pain, please contact Dr. Donald Corenman, Vail, Aspen, Denver and Grand Junction, Colorado back doctor and spine specialist, for additional information on chronic radiculopathy.