An Overview of
Three membranes, the dura mater, arachnoid and pia mater surround the spinal cord and nerves. The dura mater, which is the outer most membrane, contains the cerebral spinal fluid (CSF) and nerves or spinal cord depending upon the level of the spine. Some individuals might have heard of a dural leak. This occurs when the spinal fluid (CSF) leaks out of a small hole in the dural membrane and causes a headache. A dural leak can be caused by an injection in the spinal column such as a spinal block or from surgery. Arachnoiditis is typically not related to a dural leak, except when a blood patch to seal the leak is not injected into the appropriate location.
The “fix” to a dural leak is something called a blood patch. A small amount of blood is withdrawn from a vein and then injected into the epidural space (the space above the dura). This blood will clot and most of the time will seal this pinhole leak. In the rare case that blood is inadvertently injected into the dural space instead of the epidural space (“epi” means “above” in Latin), the blood within the dural space can cause arachnoiditis.
The pia mater is the innermost membrane that lines the actual nerves within the canal. The arachnoid is the membrane sandwiched between the dura mater and the pia mater. The arachnoid membrane (the middle layer) has hundreds of small spider web type attachments from nerve to nerve and this explains how it was named. The word “Arachnoiditis” is a combination of two words taken from the root Latin. “Arachnoid” means spider and “itis” means inflammation of. This is similar to the term “appendicitis” where this means inflammation of the appendix.
What is ?
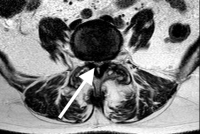
Arachnoiditis is actually the inflammation of the arachnoid membrane. The nerves are coated by this membrane within the CSF and inflammation can cause scarring and the nerves to “stick together” in clumps. Interestingly enough- like many conditions of the spine, some people have this condition and never develop symptoms.
Arachnoiditis is caused by a number of conditions. Arachnoiditis was more common in the 1970s and early 1980s when radiologists used an older type of oil based myelogram dye. This dye was used back then to visualize the spinal canal to look for canal compression and disc herniations. Thankfully- this dye is no longer used.
Arachnoiditis can be caused by the compression of spinal stenosis associated with degenerative spondylolysthesis (see section on this website). When an individual experiences back pain in the L4-L5, degenerative spondylolysthesis can often be the condition leading to the inflammation. Epidural steroids can be used to manage the pain of spinal stenosis and individuals can now live with this nerve compression of the spine associated with canal narrowing of the spine. There is however, a certain small percentage of these individuals living with stenosis that will develop arachnoiditis of the lumbar spine.
Arachnoiditis of the lumbar spine can also be caused by spinal cord trauma, infection of the spinal cord, inflammation, and even surgery. If there is a larger dural tear during surgery, there is a chance of arachnoiditis. If spinal cord trauma occurs such as in a motor vehicle accident and bleeding in the spinal canal results, arachnoiditis can form. Spinal cord trauma also includes fractures of the spine that disturb the nerves in the canal can cause this condition. Obviously infection can cause injury to the structures that have become infected and the arachnoid is no exception to this rule. Meningitis (the arachnoid is a meningie just like the dura and pia) can cause arachnoiditis. Tuberculosis is famous for causing arachnoiditis. Cancer in the central nervous system can cause arachnoiditis.
The pathology of arachnoiditis of the lumbar spine is that the small spider web connections scar, contract and stick the nerves together. This reduces the nerve membrane exposure to the CSF and injures the small blood vessels that line and feed these nerves. This lack of blood circulation and the direct scar injury to the nerve can cause chronic nerve discharge or blocked signals. The nerves also don’t move normally when scarred. A normal nerve moves back and forth in the canal up to an inch when the leg is flexed or extended just like a cable over a pulley. If the nerve is tethered, it can’t stretch and the mechanical deformation with movement can cause symptoms.
Chronic nerve membrane injuries caused by spinal cord trauma or damage to the spinal cord can cause spontaneous discharges, blocking of the signal or nerve tethering. The symptoms generated depend upon the function of the damaged nerve. If it is a proprioceptive nerve, pins and needles will result (paresthesias). If it is a motor nerve, weakness can occur. If it is a sensory nerve, numbness or even bizarre sensations can occur (hot water dripping down the leg). If it is a bowel or bladder nerve, dysfunction can occur. When aggravated, pain nerves will deliver aberrant pain signals. “Burning pain of the spine” is one of the characteristics of arachnoiditis but can be seen in any chronic nerve injury of the spine such as peripheral neuropathy or chronic radiculopathy.
Management of
Unfortunately, there is no cure for arachnoiditis- only management. Patients who have experieinced spinal cord trauma or a spinal cord injury may suffer from this condition, but thankfully, many patients who have arachnoiditis don’t even know it is present and need no treatment. However, if treatment is needed, treatment will not be curative but is designed to manage the symptoms using therapy and medications for the spine. For severe flair-ups, epidural steroids can occasionally be temporarily effective.
A chronic pain specialist normally manages patients with arachnoiditis. This expert can originate from many different specialties such as internal medicine, occupational medicine or physical medicine.
A surgically implantable spinal cord stimulator can reduce the symptoms in some patients. If a patient decides to go that route, consultation with an implant specialist that has significant experience with this condition is important.
For more information on arachnoiditis of the lumbar spine, please contact Dr. Donald Corenman, spine specialist and back doctor offering diagnostic and surgical second opinions to patients in the USA and around the world.