This syndrome involves trapping of a peripheral nerve in a tunnel. These peripheral nerves are different from the nerves in the spinal canal (the radicular nerves) due to their “protective armor”, the epineurium and perineurium. This protective sheath makes the nerve less vulnerable to injury than the spinal nerves. Nonetheless, these nerves can be injured by stretch, impact and compression.
All of these entrapment syndromes are very similar in their pathology (the basic disorder that causes the problem). This pathology is compression of the nerve by a bone or tendon. The difference in each disorder is the nerve distribution (where the nerve travels and what it does) and whether this nerve contains only sensory nerves, only motor nerves or a combination of the two.
You can read about the specifics of what causes the microscopic damage to a nerve in the separate topic “Nerve Injuries and Recovery” on this website
If the compressed nerve has strictly a pure sensory distribution, no motor weakness will be present and therefore no atrophy can occur. Atrophy only occurs when the muscle belly shrinks due to a lack of nerve supply.
However, pain inhibition can cause temporary muscle weakness in certain leg positions. This is not true muscle weakness but an actual subconscious reflex to prevent pain from occurring by subconsciously refusing to contract the muscle for fear of pain.
We will first discuss the general symptoms that can occur with peripheral nerve compression.
Sensory Symptoms
With peroneal neuropathy, the nerve becomes compressed. As pressure increases on the nerve, the blood flow decreases. This causes nerve malfunction such as conduction loss and unintended conduction called ectopic stimuli. Loss of conduction means the nerve will not convey messages to the brain from the skin. This loss of sensation is obviously described as “numbness”.
Injury can also cause conduction to occur even when the nerve is not stimulated. This is like a short circuit in doorbell wiring making the doorbell ring when no one is at the door. The patient notes these sensations as pain, paresthesias (pins and needles) as well as bizarre sensations (ants crawling or cold water splashing on the skin).
The continued crush injury can also injure the myelin sheath, the “insulation” of the nerve. This can be more of a permanent injury. Myelin sheath injuries can heal but this healing takes between 8-14 weeks for recovery.
With compression of the nerve, increased “pins and needles” (paresthesias) typically occur. Electric shock sensations (Tinel’s sign) that “zing” down the nerve then can occur. Abnormal spontaneous hot and cold sensations can develop in the distribution of the nerve
With chronic injury, fluid collects in the space that the nerve occupies and the nerve itself can swell, increasing the intensity of the symptoms. Continued nerve injury can induce pain. Burning sensation can occur when the nerve develops permanent injury. The pain can worsen and spread. Pain tends to be worse with activity and is relieved by rest but continuous pain can occur with chronic injury.
Motor Symptoms
Motor strength loss typically occurs gradually. There are rare circumstances however where the entire muscle group can fail all at once. In the leg with peroneal neuropathy, this might manifest as foot drop, the inability to hold the foot up when walking. With foot drop, the foot will slap on the ground or even “catch”: the ground when the foot swings through when walking.
As small muscles lose their nerve supply they can create a “cramping feeling”. Cramping can be an indication of weakness but other non-related disorders can also cause cramping.
Causes of Nerve Entrapment Syndromes
Most entrapment syndromes are caused by mechanical and genetic problems. Genetics have to do with the size of the tunnel these nerves travel in. Some people have congenitally smaller tunnels and with aging, previous injury, degeneration (bone spurs) and inflammation, these tunnels become crowded. Mechanically, overuse syndrome can cause tendons to swell (tendonitis and synovitis) and crowd out the nerve.
There are genetic and metabolic disease processes that can contribute to nerve malfunction. These processes may increase the swelling (crowding) of the tunnel or make the nerve itself more sensitive. These disorders include rheumatoid arthritis, hypothyroidism, pregnancy, diabetes, acromegaly (too much human growth hormone) and CMT syndrome (Charcot Marie Tooth syndrome-a genetic condition).
Common Peroneal Nerve Entrapment Syndrome
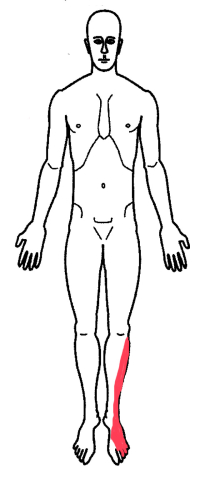
The sciatic nerve splits into two nerves as it descends into the leg. Just above the knee, these split nerves are called the common peroneal nerve and tibial nerve. The common peroneal nerve then splits into the deep and superficial peroneal nerves right at the fibular head, the bone on the bottom outside of the knee joint.
To go back to anatomy, the lower leg has two bones, the tibia and fibula. The tibia is the main bone of the lower leg and makes up the bottom surface of the knee joint. The fibula is the smaller bone on the outside of the leg and acts as a strut rod, a stabilizer bone for the leg. It is this bone that the peroneal nerve wraps around.
The peroneal nerve is very superficial here (right under the skin) and exposed to potential injury. Injury can occur from impact (falling off a bicycle) or by being struck by a blunt object (a ski or hockey stick). Other actions that can injure the nerve are surgery (knee joint replacement or fracture) and even the chronic act of crossing the legs while sitting. Continuous wearing of high boots with tops that rest against the outside of the leg in this region or the use of ski boots can even set this injury off.
Symptoms
This nerve supplies both motor and sensory fibers to the leg. The sensory portion of the nerve supplies the outside of the shin and the top of the foot (but not the first two toes). This region of the leg and foot will develop numbness and paresthesias (pins and needles). This is noted especially if the outside of the knee where the nerve was located (the fibular head) was struck by an object or continuous pressure was applied (crossing the legs). If symptoms are severe, the numbness can wake the patient up from a dead sleep.
The motor portion of the nerve supplies the muscles of the anterior and lateral aspect of the shin. These muscles are responsible for lifting the foot up when walking and preventing the foot from turning in when weighting the leg.
Motor nerve injury would then cause two particular symptoms of weakness, foot drop and inversion sprain. Foot drop occurs when walking. The foot will slap on the ground when the heel strikes the surface. Occasionally, the toes of the foot will “catch” the ground when the leg pushes forward and the patient can “trip over their own foot”.
The other noticeable weakness will be the “feeling” of the ankle wanting to “turn in” similar to the feeling of being on the verge of “spraining the ankle”. This is due to weakness of the ankle evertors, the peroneal muscles which prevent the foot from “turning in”.
Diagnosis
History, examination and special testing confirm the diagnosis of this condition. The history is exactly like that noted above.
L5 nerve compression in the spinal canal from a herniated disc can look very similar to peroneal neuropathy so great care has to be used to differentiate peroneal nerve compression (rare) from L5 radiculopathy (common).
Testing essentially consists of one or two tests. The Tinel’s test has to do with the exquisite sensitivity of any nerve at an injury point. A nerve that is injured will fire an ectopic focus (a lightening bolt of electricity) down to the end of nerve when stimulated. Percussion of the injury area will elicit this “lightening bolt”. In the case of peroneal fibular head entrapment syndrome, the injury point is where the nerve wraps around the fibula. A positive test will cause an electrical “zap” into the foot with percussion of the peroneal nerve at this location.
Some physicians will perform a two-point discrimination test. This test uses the ends of monofilament fishing line on a tool that can separate these two points at a specific distance. This tool is used to determine the smallest distance that a patient can identify the distance between these two points. In peroneal nerve/fibular head entrapment syndrome, this distance will be larger than normal in the outside of the shin as the sensitivity of the skin here diminishes.
Finally, an electrical test called an EMG/NCV can be used to determine if there is conduction loss or muscle weakness. A negative test (no findings) would not preclude a diagnosis of peroneal nerve/fibular head entrapment syndrome.
Treatment
Treatment depends upon the severity of the symptoms. Intermittent symptoms that do not bother the patient and do not wake them up at night generally do not need to be treated.
With increasing symptoms, medications such as NSAIDs (Motrin, Aleve) can be helpful. Steroid injections can rarely give relief.
If symptoms continue without relief or motor weakness occurs, surgical decompression of the nerve can provide long-term relief.